Medex
Ahmad Adi, MD
- Department of Cardiothoracic Anesthesiology
- Cleveland Clinic
- Cleveland, Ohio
By definition hiv infected macrophages purchase medex us, interfering factors lead to measuring results that do not correspond to the actual in vivo concentration of the sought-after analyte natural factors antiviral echinamide buy 1mg medex mastercard. A basic differentiation should be made between a) the influence or loss of a test reaction as a result of interfering factors and b) reactions that are caused by cross-reactions or polyclonal stimulations which can induce false-positive results hiv infection gif buy generic medex pills. False-negative or erroneously low results can also be caused by incomplete antibodies or very high antibody concentrations in the sample (prozone phenomenon) antiviral supplements order cheap medex. The latter can induce competition between the analyte and the antigens used in the test hiv infection rates by race purchase medex 5 mg fast delivery, and antiviral brandon cronenberg medex 5 mg lowest price, thus, lead to an impairment of the antigen antibody bond. These can lead to a strong (mostly bluish) background color on immunoblot strips. Detailed information on pathogen and/or test-specific interfering and influencing factors is listed in the respective pathogen sections. Cross reactivity is when antibody detection is troubled because the (antibody-specific) antigen is similar to the antigens of a (sometimes) closely related pathogen with a similar antigen structure. Therefore, results that are solely IgM positive should always be viewed with caution, particularly as they can cause increased psychological strain in patients in this situation. Of the more than 35 known species of the genus Actinomyces, around 20 are relevant for human medicine. They are also found in the urogenital tract and on the skin of healthy individuals. Actinomycetes are much more commonly found in polymicrobial processes, such as dental abscesses, brain abscesses, para-rectal abscesses etc. Immunoassays for detecting specific antibodies against Actinomyces species are not available. Furthermore, antibodies against Actinomyces viscosus have been detected in 16%, and antibodies against A. As part of the diagnostic testing for periodontitis, studies have detected antibodies against periodontitis-associated bacteria, including Actinomyces spp. The informative value of this serology is, however, not proven for this indication. The detection of IgG antibodies against thermophile actinomycetes in the environment, such as Micropolyspora spp. They only grow after a long incubation period under microaerophilic conditions on special culture media. There is a very close phylogenetic relationship between rickettsia and brucella [166; 171]. Trench fever has recently experienced a Renaissance, affecting individuals living in poor hygienic conditions. In addition to local infections, systemic progression with organ-related manifestations of sepsis can also occur. Papulopustular efflorescence and regional swelling of the lymph nodes occur at the entry point after approximately 7 days. In periodic forms of the disease, recurring bouts of fever can last for several days; in chronic forms, fever can persist for several weeks. After the general infection, patients, even those who are not immunosuppressed, experience knotty angiomatosis of the skin that can sometimes persist for years 46 (verruga peruana). Furthermore, Bartonella are also known to trigger fevers of unclear origin, endomycarditis, eye infections and neurological infections. Cultivation is only possible in special laboratories which is why indirect pathogen detection using antibody testing is of major importance [117; 156]. If there is a clinical indication, indirect pathogen detection through antibody testing can be attempted after the first or second week of illness. A class-specific detection of the immune response for IgG, IgA and IgM is possible for all test systems. When whole cell antigens are used, it should be noted that different culture conditions can influence the antigen expression of the bartonella [171]. Antigen preparations based on cell culture have proven to be particularly suitable. Specific IgM antibodies peak at around 4 weeks and fall to below the detection threshold within 100 days. IgA antibodies also form and are considered to be an indication of an existing or recent infection. IgM antibodies can persist longer in chronic forms of the disease; however, only IgG detection has been diagnostically established in routine diagnostic testing. In contrast, depending on the test system, there is insufficient standardization with regard to IgM and IgA detection [171; 335]. For specific IgG detection, titers between 64 and 128 are considered to be an indication of an existing or recent bartonella infection. However, clinically ill patients without immune suppression exhibit much higher titers. A quadrupling of the titers in samples collected during the course of the infection and tested in parallel, and/or the diagnosis of a seroconversion, are evidence of a fresh infection. However, seronegative results for clinically and microbiologically ascertained bartonellosis have not only been identified in immune-suppressed patients [335; 171]. Cross-reactivities also exist with treponema, chlamydia, mycoplasma, coxiella, ehrlichia, anaplasma, bordetella, francisella, and toxoplasma, i. Therefore, positive results of bartonella serology should always be interpreted with caution, taking into account the clinical context. They require critical scrutiny for the tests used in the respective labs and should undergo a lab-internal performance test on positive reference samples and negative blood donor sera depending on the local epidemiological situation. The detection of IgA and IgM antibodies is of little value and should only be regarded as an additional procedure. A negative test therefore does not eliminate bartonellosis, particularly since seronegative bartonellosis does occur. The possible causes of false-reactive findings are often due to a variety of cross reactivities. If the clinical symptoms are unclear or severe, molecular detection in tissue samples is recommended for further confirmation. In countries with a high vaccination coverage for infants and toddlers, non-vaccinated or insufficiently vaccinated infants, as well as older children, adolescents and adults become ill. In recent years there has been an increase in pertussis-related illnesses in adults in the second half of life as a result of a deficient booster after the age of 30. The latter phenomenon also plays an important role in the spread of the pathogen to unprotected infants. The disease is contracted by up to 90% of individuals in close contact after initial contact; contagiousness appears to be lower with subsequent contact [239]. Pneumonia is often a complication of whooping cough and responsible for half of the deaths resulting from a pertussis infection. Values between 40 and 100 could indicate a recent or past infection, however this should be clarified through further testing. An immune response after a vaccination cannot be distinguished from one following an infection. IgA antibodies against Bordetella-specific antigens can also be detected after vaccinations. Therefore, pertussis serology cannot be assessed with certainty for at least one year after vaccination with an acellular vaccine. No differentiation between antibody formation after vaccination or after infection is possible. The measurable antibody concentrations do not allow for any conclusions to be drawn regarding existing protection or the length of immunity after vaccination. In contrast to other spirochete treponemas they are longer, have irregular spirals and can be colored with aniline dyes [34; 151]. The pathogens of human Lyme borreliosis in Germany include Borrelia burgdorferi, B. The pathogens of Lyme borreliosis are transmitted to humans by hard-bodied ticks (Ixodes species), making Lyme borreliosis one of the more important vector-transmitted infectious diseases in the northern hemisphere. The number of new cases in Germany is estimated to be between 60, 000 and 200, 000 per year [151; 219]. The majority of patients are infected between the end of April and the end of September by ticks that are particularly active during this period. Typical places where infection occurs are the edges of forests and pathways, parks, shrubs, and gardens with undergrowth. The probability of transmission increases with the length of blood feeding and, depending on th th the regional epidemiology, only every 100 to 1000 tick bite results in an infection [34; 151]. Tick borne relapsing fever is endemic to certain regions around the world and is transmitted in Europe by 50 argasidae, particularly in eastern and southern Europe. This is combined with typical, repeated bouts of fever with alternating fever-free intervals. The illness is particularly regarded as a travel infection affecting people who are returning from endemic areas and asylum seekers [34]. The clinical picture of Lyme borreliosis, which is much more significant in this country from an infectiology point of view, is manifold and the incubation period can last weeks to months. The manifestations of the disease are divided into early manifestations and late manifestations. Leading symptoms include radicular pain syndrome (an agonizing, burning pain that particularly occurs at night) and/or cranial nerve paralyses (particularly of the N. Late manifestations include acrodermatitis chronica atrophicans, chronic arthritis and, more seldom, polyneuropathic manifestations (in association with acrodermatitis chronica atrophicans) and chronic encephalomyelitis [34; 151; 300]. Direct detection using microscopy and, where possible, molecular biological methods, is crucial for relapsing fever Borrelia. In contrast, antibody detection plays no fundamental role in diagnosing relapsing fever Borrelia in diagnostic practice [34; 151]. By contrast, indirect serological pathogen detection plays a critical role in diagnosing Lyme borreliosis. In accordance with valid procedures in Germany, a stepwise approach to diagnostic testing is used to detect antibodies. The use of a variety of recombinant immunodominant proteins from different Borrelia spp. Even though the principle testing procedures and the interpretation of serological test results are standardized in Germany [114], the different test systems vary considerably and are subject to manufacturer-related differences in the accurate interpretation of test results or the interpretation criteria for specific immunoblot bands [151; 158; 219]. Around 50% of patients with erythema migrans and around 20% of patients with disseminated early manifestations are, therefore, initially seronegative. When the disease manifestation is unequivocal (classic erythema migrans), the need for serological tests and control tests is not indicated [151; 300]! After successful treatment or after the infection has healed, the antibody response regresses very slowly so that IgM antibodies can remain detectable for months or years under certain circumstances [34; 151]. Therefore, the IgM antibody result is of limited diagnostic value, particularly since a specific IgG response is detected early on by introducing very specific VlsE antigens to the test procedure. Even positive IgG findings can persist at higher titers for longer periods of time. The immune response can be divided into an early and a late phase for the purpose of orientation in order to improve correlation with clinical symptoms.
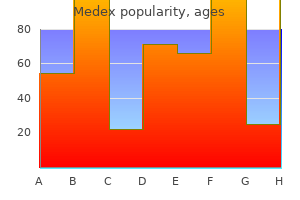
Laundry staff should protect themselves from potential cross-infection from soiled linen by wearing appropriate protective equipment hiv infection swollen lymph nodes buy generic medex online, such as gloves and gowns or aprons time between hiv infection and symptoms order medex in united states online, when handling soiled linens hiv bladder infection symptoms order medex uk. Laundry staff should be trained in procedures for safe handling of soiled linen and must be 10 hiv infection rate condom cheap medex online mastercard, 44 offered immunization against hepatitis B hiv infection symptomatic stage 1 mg medex otc. Waste Written policies and procedures for management of contaminated infectious waste from health care settings must be developed based on provincial regulations and local bylaws and should address issues such as the collection hiv infection ppt buy medex 5mg lowest price, storage, transport, handling and disposal of contaminated waste, including sharps and biomedical 10 waste. Waste handlers who may be exposed to biomedical waste and/or sharps must be offered hepatitis B immunization. Where infection risks cannot be eliminated or substituted, engineering controls are the preferred next choice for controlling the risk, because they are built into the facility infrastructure and do not rely on individuals to implement them correctly. A sharps injury prevention program must be in place in all health care 11, 16 77 settings. There is a regulatory requirement to inspect the mechanical ventilation system (including airborne 79 infection isolation rooms) every six months to ensure it is in good condition. Respiratory Etiquette Health care settings should reinforce with staff, clients/patients/residents and visitors the personal practices that help prevent the spread of microorganisms that cause respiratory infections. These personal practices include: not visiting in a health care facility when ill with an acute respiratory infection avoidance measures that minimize contact with droplets when coughing or sneezing, such as: turning the head away from others 47 maintaining a two-metre separation from others covering the nose and mouth with tissue immediate disposal of tissues into waste after use immediate hand hygiene after disposal of tissues. Healthy Workplace Policies All health care settings should establish a clear expectation that staff do not come into work when ill with symptoms that are of an infectious origin, and support this expectation with appropriate 68 attendance management policies. All health care settings should have an age 11 appropriate immunization program in place. Staff Immunization Immunization programs are highly effective and are a critical component of the occupational health and 83, 84 safety program. Appropriate vaccine use protects the health care provider, colleagues and the client/patient/resident. Incorporate the elements of Routine Practices into the culture of all health care settings and into the daily practice of each health care provider during the care of all clients/patients/residents at all times. Wear gloves when it is anticipated that the hands will be in contact with mucous membranes, non intact skin, tissue, blood, body fluids, secretions, excretions, or equipment and environmental surfaces contaminated with the above. Ensure that there is a clear expectation that staff do not come into work when ill with symptoms that are of an infectious origin, and this expectation is supported with appropriate attendance management policies. Additional Cleaning Measures Additional cleaning measures may be required for the client/patient/resident environment. Cohorting should never compromise infection control practices and Additional Precautions must be applied individually for each client/patient/resident within the cohort. Rather, those who already share a room or who share a bathroom and who are infected or colonized with the same microorganism may be treated as a cohort. Use of this practice can limit transmission by segregating those who are infected or colonized to a specified area away from those 96 who are not. Staff Cohorting Staff cohorting is the practice of assigning specified health care providers to care only for clients/patients/residents known to be colonized or infected with the same microorganism. This practice can be used during outbreaks to reduce the potential for cross-infection between clients/patients/residents by limiting the number of staff interacting with 97-99 clients/patients/residents. Clients/patients/residents and visitors must be informed about the reason for implementing Additional Precautions and receive instruction regarding how to enter and leave the room safely when the client/patient/resident is on Additional Precautions. Initiation of Additional Precautions Additional Precautions must be instituted as soon as symptoms suggestive of a transmissible infection are noted, not only when a diagnosis is confirmed (see Table 2 for examples). Abscess or draining wound not contained by dressing Contact Yes Diarrhea and/or vomiting of suspected acute Contact Yes infectious etiology Rash Suggestive of varicella or measles Airborne Yes, with negative air flow and door closed. The attending physician should be notified when Additional Precautions are being discontinued. Health care settings should have policies that authorize the Infection Prevention and Control Professional to initiate and/or discontinue Additional Precautions. Recent studies, however, have noted that patients on Contact Precautions did not perceive a negative 81, 110 81 impact on their care, and often perceived precautions as an improvement in their care. Some 107 patients valued the privacy and solitude afforded by Contact Precautions and the quietness and 108 privacy of single rooms. Psychological support for the client/patient/resident should include structured recreation programs, steps to prevent time disorientation and psychological support for both clients/patients/residents and 81, 101, 103, 108, 111-113 their families. Clients/patients/residents should be encouraged to perform hand hygiene on arrival in, and departure from, an ambulatory/clinic setting. If single rooms are unavailable, clients/patients/residents may be cohorted with other clients/patients/residents who are infected with the same microorganism. In long-term care and other residential settings, placement of residents requiring Contact Precautions 18 should be reviewed on a case-by-case basis. Infection risk to other occupants of the room must be considered when selecting roommates. It is never appropriate for clients/patients/residents to wear gloves or isolation gowns while outside their room. Recent work suggests that droplets forcibly expelled from a cough or sneeze travel for up to two metres 126, 127 or more, depending on the amount of air turbulence in the immediate vicinity. Contact transmission can then occur by touching surfaces and objects contaminated 8 with respiratory droplets. Examples of microorganisms transmitted by droplet transmission include: respiratory tract viruses. Figure 6: Droplet transmission from coughing or sneezing Elements that Comprise Droplet Precautions In addition to Routine Practices, the elements that comprise Droplet Precautions are summarized in Table 4. Clients/patients/residents must perform hand hygiene on presentation and departure from an ambulatory/clinic setting. Accommodation Preferred accommodation for Droplet Precautions in acute care is a single room with a dedicated toilet and patient sink, and door may remain open. Transport In most cases, transport should be limited unless required for diagnostic or therapeutic procedures, such 55 as ambulation. If the client/patient/resident cannot tolerate wearing a mask, transport staff should wear a mask and eye protection. Airborne Transmission Airborne transmission occurs when airborne particles remain suspended in the air, travel on air currents and are then inhaled by others who are nearby or who may be some distance away from the source patient, in a different room or ward (depending on air currents) or in the same room that a patient has 8 left, if there have been insufficient air exchanges. Effective control of airborne microorganisms hinges on maintaining a high degree of suspicion for those 128 who present with compatible symptoms of an airborne infection, early isolation in an appropriate environment and rapid diagnosis. Controls for preventing the transmission of airborne infections include: immunity against measles and varicella early identification of potential cases prompt isolation in an airborne infection isolation room appropriate treatment of client/patient/resident, where applicable the use of a fit-tested, seal-checked N95 respirator, when indicated identification and follow-up of exposed clients/patients/residents and staff. Elements that Comprise Airborne Precautions N95 Respirators A fit-tested, seal-checked N95 respirator must be worn by all staff when entering the room, 129 transporting or caring for a client/patient/resident with signs and symptoms or a diagnosis of active pulmonary or laryngeal tuberculosis. Client/Patient/Resident Controls Patients on Airborne Precautions should remain in the airborne infection isolation room unless required to leave for medical reasons. For varicella and measles: Household contacts of patients with measles or varicella are not required to wear an N95 respirator when visiting, as they will already have been exposed in the household. Recommended Engineering Controls for Reducing Transmission of Microorganisms Spread by the Airborne Route Engineering controls. At a minimum, the emergency room, bronchoscopy suites, critical care settings and autopsy suites must have rooms with negative pressure capabilities as described above for high risk procedures. In acute settings expected to care for patients with infectious pulmonary tuberculosis, measles, varicella or disseminated zoster, a sufficient number of negative pressure rooms must be available on in-patient units. An assessment of the risk of exposure to airborne infections will assist in establishing the location and number of airborne infection isolation rooms required in order to decrease the risk of exposure to airborne infections in the health care setting. Preferably this should be a negative pressure room with exhaust vented to the outside or filtered through a high efficiency filter if recirculated. Where more than one mode of transmission exists for a particular microorganism, the precautions used must take into consideration both modes. These microorganisms may be transmitted by contact as well as by droplet transmission and, therefore, both 8, 18 Contact and Droplet Precautions are required. If both tuberculosis and a respiratory virus are suspected in a single individual, a combination of Airborne, Droplet and Contact Precautions should be used. It is critical that health care providers and others who are acutely ill with a communicable infection do not enter the room of immunocompromised patients. When single patient rooms are limited, determine the feasibility of cohorting patients who are infected or colonized with the same microorganism. In ambulatory settings, place patients who require Contact Precautions in an examination room or cubicle as soon as possible. Remove gloves and perform hand hygiene immediately on leaving the room or bed space. In non-acute settings, for Contact Precautions wear gloves and a gown for activities that involve direct care. Whenever possible, dedicate equipment and items to the client/patient/resident on Contact Precautions. In acute care, place patients who require Droplet Precautions in a single room with dedicated toilet and patient sink, when available. Triage symptomatic client/patient away from waiting area to a single room as soon as possible, or maintain a two-metre spatial separation. Move clients/patients/residents who require Airborne Precautions to an airborne infection isolation room as soon as possible. Wear an N95 respirator when entering an airborne infection isolation room when it is being used for tuberculosis. Do not enter the room of a patient with measles, varicella or zoster unless immune. All health care providers have a responsibility to know their immunization status (see Section 2. Staff who consume food or beverages in care areas (client/patient/resident environment, nursing station, charting areas) are at increased risk for acquiring serious foodborne gastrointestinal infections. Institutional 139-144 145 outbreaks involving staff have been reported, particularly with hepatitis A, cryptosporidiosis and 146 norovirus. There should be a program to deal with staff exposures that includes: identification of exposed staff assessment and immunization history post-exposure prophylaxis and follow-up including: collection and analysis of exposures 16, 77 a program for prompt response to sharps injuries policies to deal with spills and staff exposure to blood or body fluids education regarding preventive actions that may be put into place to improve practices and prevent recurrence. Health care providers must receive training on how to perform a 8, 129, 131, 132 seal-check correctly in order to obtain a tight facial seal. Non-compliance should not be tolerated, as this is a patient and health care provider safety issue. Wear gloves when it is anticipated that the hands will be in contact with mucous membranes, non-intact skin, tissue, blood, body fluids, secretions, excretions, or equipment and environmental surfaces contaminated with the above. Single rooms, with dedicated bathroom and sink, are preferred for placement of all clients/patients/residents. Provide clear protocols for determining options for patient placement and room sharing based on a risk assessment if single rooms are limited. Place clients/patients/residents who visibly soil the environment or for whom appropriate hygiene cannot be maintained in single rooms with dedicated toileting facilities. Implement a program that promotes respiratory etiquette to staff, clients/patients/residents and visitors in the health care setting. When cohorting, apply Additional Precautions individually for each client/patient/resident within the cohort. Do not wear the same gowns and gloves when going from patient-to-patient within the cohort and do not share patient care equipment. In all health care settings, implement a policy authorizing any regulated health care professional to initiate the appropriate Additional Precautions at the onset of symptoms. In long-term care and other residential settings, place residents who require Contact Precautions as determined on a case-by-case basis using a risk assessment. If used, remove gown and perform hand hygiene immediately on leaving the room or bed space. Restrict client/patient/resident on Airborne Precautions to his/her room with the door closed, unless he/she must leave the room for medically necessary procedures. Wear an N95 respirator during transport of clients/patients/residents on Airborne Precautions. C Insufficient evidence to support a recommendation for or against use D Moderate evidence to support a recommendation against use. Intervention and Interaction #1: I must follow Routine Practices because there is a risk that I might expose myself Individual Risk Assessment #1 to an infection that is transmitted via this route, or expose the client/patient/resident to my Decision #2: Do I need protection for microorganisms (see algorithms) what I am about to do because the client/patient/resident has undiagnosed symptoms of infection Intervention and Interaction #3: I must follow the procedures proscribed Organizational Risk Assessment for this infection to protect myself and others (see Appendix N). If yes: Should be accommodated preferentially in a single room If a single room is not available, maintain a spatial separation of at least two metres Facial protection for close contact with the client/patient/resident Initiate Contact Precautions if indicated. Gown [based on risk assessment] Wear a long-sleeved gown if contamination of skin or clothing is anticipated. Linen and Waste Handle soiled linen and waste carefully to prevent personal contamination and transfer to other clients/patients/residents. Paediatric* and Contact Yes Continue precautions incontinent/non for duration of illness.
Viruses of the same group cause similar infections in many animal species but are of minor importance as sources of human infections antiviral ilaclar purchase cheapest medex and medex. Viruses discharged in the feces hiv infection statistics in south africa medex 1 mg for sale, including enteroviruses and adenoviruses antiviral que son cheap medex uk, may be transmitted by the fecal-oral route primary hiv infection symptoms rash buy medex from india. Outbreaks of illness due to adenovirus types 3 hiv infection unaids cheap medex 1 mg visa, 4 and 7 have been related to swimming pools hiv infection rates prostitutes cheap 1 mg medex fast delivery. Individu als with compromised cardiac, pulmonary or immune systems are at increased risk of severe illness. Outside hospitals, ill people should avoid direct and indirect exposure of young children, debilitated or aged people or patients with other illnesses. Indiscriminate use of antibiotics is to be discouraged; they should be reserved for patients with group A streptococcal pharyngitis and patients with identi ed bacterial complications such as otitis media, pneumonia or sinusitis. Cough medicines, decon gestants and antihistaminics are of questionable effectiveness and may be hazardous, especially in children. Some nosocomial transmission can be prevented by good infection control procedures, including handwashing; procedures such as ultraviolet irradiation, aerosols and dust control have not proven useful. They are transmitted by ixodid (hard) ticks, which are widely distributed throughout the world; tick species differ markedly by geographical area. For all of these rickettsial fevers, control measures are similar, and doxycycline is the reference treatment. A maculopapular rash generally appears on the extremities on the 3rd to 5th day; this soon includes the palms and soles and spreads rapidly to much of the body. A petechial exanthem occurs in 40% to 60% of patients, generally on or after the 6th day. Risk factors associated with more severe disease and death include delayed antibio therapy and patient age over 40. Absence or delayed appearance of the typical rash or failure to recognize it, especially in dark-skinned individu als, contribute to delay in diagnosis and increased fatality. The rickettsiae can be transmitted to dogs, various rodents and other animals; animal infections are usually subclinical, but disease in rodents and dogs has been observed. Contamination of breaks in the skin or mucous membranes with crushed tissues or feces of the tick may also lead to infection. Chloramphenicol may also be used, but only when there is an absolute contraindication for using tetracyclines. Treatment should be initiated on clinical and epidemiological considerations without waiting for laboratory conrmation of the diagnosis. Expansion of the European endemic zone to the north occurs because tourists often carry their dogs with them; the dogs acquire infected ticks, which establish colonies when the dogs return home, with subsequent transmission. In more temperate areas, the highest incidence is during warmer months when ticks are numerous; in tropical areas, disease occurs throughout the year. Clinically similar to Boutonneuse fever (see above), but fever less com mon, rash noticed in only half the cases and may be vesicular. Multiple eschars, lymphangitis, lymphadenopathy, and oedema localized to the eschar site are seen more commonly than with Boutonneuse fever. Outbreaks of disease may occur when groups of travellers (such as persons on safari in Africa) are bitten by ticks. Ixodes holocyclus, which infests small marsupials and wild rodents, is probably the major vector. An initial skin lesion at the site of a mite bite, often associated with lymphadenopathy, is followed by fever; a disseminated vesicular skin rash appears, which generally does not involve the palms and soles and lasts only a few days. The disease, caused by Rickettsia akari, a member of the spotted fever group of rickettsiae, is transmitted to humans from mice (Mus musculus) by a mite (Liponyssoides sanguineus). Incidence has been markedly reduced by changes in management of garbage in tenement housing, so that few cases have been diagnosed in recent years. Clinically, this is usually indistinguish able from febrile rash illness due to measles, dengue, parvovirus B19, human herpesvirus 6, Coxsackie virus, Echovirus, adenovirus or scarlet fever. Leukopenia is common and throm bocytopenia can occur, but hemorrhagic manifestations are rare. Arthral gia and, less commonly, arthritis complicate a substantial proportion of infections, particularly among adult females. Encephalitis is a more common complication than generally appreciated, and occurs with a higher frequency in adults. Laboratory diagnosis of rubella is required, since clinical diagnosis is often inaccurate. An epidemiologically conrmed rubella case is a patient with suspected rubella with an epidemiological link to a laboratory conrmed case. Rubella is important because of its ability to produce anomalies in the developing fetus. Congenital malforma tions and fetal death may occur following inapparent maternal rubella. Fetuses infected early are at greatest risk of intrauterine death, sponta neous abortion and congenital malformations of major organ systems. In countries where rubella vaccine has not been introduced, rubella remains endemic. By the end of 2002, 124 countries/territories (58% of the world total) were using rubella vaccine in their national immunization program with the highest levels in the Americas (94% of countries), Europe (84%) and the Western Pacic (59%). Preventive measures: 1) Educate the general public on modes of transmission and stress the need for rubella immunization. Consequently, it is essential that childhood rubella vaccination programs achieve and maintain high levels of coverage (above 80%) on a long-term basis. Following the introduction of large-scale rubella vacci nation, coverage should be measured periodically by age and locality. If resources permit, longitudinal serological surveillance can be used to monitor the impact of the immunization program, especially through assessing ru bella IgG antibody in serum samples from women attend ing antenatal clinics. Rubella vaccine should be avoided in pregnancy be cause of the theoretical, but never demonstrated, terato genic risk. If pregnancy is being planned, then an interval of one month should be observed after rubella immunization. Rubella vaccine should not be given to anyone with an immunodeciency or who receives immunosuppressive therapy. In case of infection with wild rubella virus early in preg nancy, culturally appropriate counselling should be pro vided. It is sometimes given in huge doses (20 ml) to a susceptible pregnant woman exposed to the disease who would not be in a position to consider abortion, but the value of this has not been established. Early reporting of sus pected cases will permit early establishment of control measures. Such contacts should be tested serologically for suscep tibility or early infection (IgM antibody) and advised accord ingly. Infection may begin as acute enterocolitis and develop into septicemia or focal infection. Occasionally, the infectious agent may localize in any tissue of the body, produce abscesses and cause septic arthritis, cholecystitis, endocarditis, meningitis, pericarditis, pneumonia, pyoderma or pyelonephritis. Deaths are uncom mon, except in the very young, the very old, the debilitated and the immunosuppressed. In cases of septicemia, Salmonella may be isolated on enteric media from feces and blood during acute stages of illness. In cases of enteroco litis, fecal excretion usually persists for several days or weeks beyond the acute phase; administration of antibiotics may not decrease this duration. Numerous serotypes of Salmonella are pathogenic for both animals and people (strains of human origin that cause typhoid and paratyphoid fevers are presented in a separate chapter). There is much variation in the relative prevalence of different serotypes from country to country; in most countries that maintain Salmonella surveillance, Salmonella enterica subsp. In most areas, a small number of serotypes account for the majority of conrmed cases. Salmonellosis is classied as a foodborne disease because contaminated food, mainly of animal origin, is the predominant mode of transmission. Only a proportion of cases are recognized clinically; in industrialized countries as few as 1% of clinical cases are reported. Epidemiologically, Salmonella gastroenteritis may occur in small outbreaks in the general population. This includes contaminated raw and undercooked eggs/egg products, raw milk/milk products, contaminated water, meat/meat prod ucts, poultry/poultry products. In addition, pet turtles, iguanas and chicks, and unsterilized pharmaceuticals of animal origin are potential sources of infection. Several outbreaks of salmonellosis have been traced to con sumption of raw fruits and vegetables that were contaminated during slicing. Infection is transmitted to farm animals by feeds and fertilizers prepared from contaminated meat scraps, tankage, sh meal and bones; the infection spreads by bacterial multiplication during rearing and slaughter. Person-to-person fecal-oral transmission is important, especially when diarrhea is present; infants and stool-incontinent adults pose a greater risk of transmission than do asymptomatic carriers. With several serotypes, a few organisms ingested in vehicles that buffer gastric acid can suffice to cause infection, but over 100 to 1000 organisms are usually required. Epidemics are usually traced to foods such as processed meat products, inadequately cooked poultry/poultry products; uncooked or lightly cooked foods containing eggs/egg products, raw milk and dairy products, including dried milk, and foods contaminated by an infected food handler. Epidemics may also be traced to foods such as meat and poultry products processed or prepared with contaminated utensils or on work surfaces contaminated in previous use. The organisms can multiply in a variety of foods, especially milk, to attain a very high infective dose; temperature abuse of food during its preparation and cross-contamination during food handling are the most important risk factors. Hospital epidemics tend to be protracted, with organisms persisting in the envi ronment; they often start with contaminated food and continue through person-to-person transmission via the hands of personnel or contaminated instruments. Maternity units with infected (at times asymptomatic) infants are sources of further spread. In recent years, geographically widespread outbreaks due to ingestion of tomatoes or melons from single suppliers have been recognized. A temporary carrier state occasionally continues for months, especially in infants.
Initial studies in Guandong Province hiv infection rates us 2012 order cheap medex on-line, China antiviral x anticoncepcional buy genuine medex line, showed similar coronaviruses in some animal species sold in markets and further study continues anti viral throat spray buy medex 1 mg amex. Initial studies suggest that transmission does not occur before onset of clinical signs and symptoms hiv infection rates with condom medex 1mg low cost, and that maximum period of communicabil ity is less than 21 days hiv time between infection symptoms generic 5 mg medex amex. Health workers are at great risk hiv transmission facts statistics cheapest medex, especially if involved in pulmonary procedures such as intubation or nebulization, and serve as a major entry point of the disease into the community. Because of the small numbers of cases reported among children, it has not been possible to assess the inuence of age. Soiled gloves, stethoscopes and other equipment must be treated with care as they have potential to spread infection. Disinfectants such as fresh bleach solutions must be widely available at appropriate concentrations. If an independent air supply is not feasible, air condi tioning should be turned off and windows opened (if away from public places) for good ventilation. Surfaces should be cleaned with broad spectrum disinfectants of proven antiviral activity Movement of patients outside the isolation unit should be avoided. Visits should be kept to a minimum and personal preventive equip ment used under supervision. Handwashing is crucial and access to clean water essential with handwashing before and after contact with any patient, after activities likely to cause contamination, and after remov ing gloves. Alcohol-based skin disinfectants can be used if there is no obvious organic material contamination. Particular attention should be paid to interventions such as use of nebulizers, chest physiotherapy, bronchoscopy or gas troscopy and other interventions that may disrupt the respira tory tract or place the healthcare worker in close proximity to the patient and to potentially infected secretions. From current epidemio logical evidence, a contact is a person who cared for, lived with, or had direct contact with the respiratory secretions, body uids and/or excretion. Use full personal protection equipment for collection of specimens and for treatment/interventions that may cause aerosolization, such as the use of nebulisers with a broncho dilator, chest physiotherapy, bronchoscopy, gastroscopy, any procedure/intervention that may disrupt the respiratory tract. Ribavirin with or without use of steroids has been used in several patients, but its effectiveness has not been proven and there has been a high incidence of severe adverse reactions. It has been proposed that a coordinated multi-centered approach to establishing the effectiveness of ribavirin therapy and other proposed interventions be examined. Place under active surveillance for 10 days and recom mend voluntary isolation at home and record temperature daily, stressing to the contact that the most consistent rst symptom that is likely to appear is fever. Ensure contact is visited or telephoned daily by a member of the public health care team to determine whether fever or other signs and symptoms are developing. Ensure adequate triage facilities and clearly indicate to the general public where they are located and how they can be accessed. Disaster Implications: As with other emerging infections, severe adverse economic impact and socio-economic consequences have been shown to occur. A global response facilitating the work and exchange of information among scientists, clinicians and public health experts has been shown to be effective in providing information and effective evidence-based policies and strategies. In typical cases, the stools contain blood and mucus (dysentery) resulting from mucosal ulcerations and conuent colonic crypt microab scesses caused by the invasive organisms; many cases present with a watery diarrhea. Severity and case-fatality rate vary with the host (age and pre-existing nutritional state) and the serotype. Shigella dysenteriae 1 (Shiga bacillus) spreads in epidemics and is often associated with serious disease and complications including toxic megacolon, intestinal perforation and the hemolytic uraemic syndrome; case-fatality rates have been as high as 20% among hospitalized cases even in recent years. Isolation of Shigella from feces or rectal swabs provides the bacterio logical diagnosis. Outside the human body Shigella remains viable only for a short period, which is why stool specimens must be processed rapidly after collection. Infection is usually associated with large numbers of fecal leukocytes detected through microscopical examination of stool mucus stained with methylene blue or Gram. Groups A, B and C are further divided into 12, 14, and 18 serotypes and subtypes, respectively, designated by arabic numbers and lower case letters. A specic virulence plasmid is necessary for the epithelial cell invasiveness manifested by Shigellae. Shigellosis is endemic in both tropical and temperate climates; reported cases represent only a small proportion of cases, even in developed areas. The geographical distribution of the 4 Shigella serogroups is different, as is their pathogenicity. More than one serotype is commonly present in a community; mixed infections with other intestinal pathogens also occur. Infection may occur after the ingestion of contaminated food or water as well as from person to person. Individuals primarily responsible for transmission include those who fail to clean hands and under ngernails thoroughly after defecation. They may spread infection to others directly by physical contact or indirectly by contaminating food. Water and milk transmission may occur as the result of direct fecal contamination; ies can transfer organisms from latrines to uncovered food items. Asymptomatic carriers may transmit infection; rarely, the carrier state may persist for months or longer. Appropriate antimicrobial treat ment usually reduces duration of carriage to a few days. The elderly, the debilitated and the malnourished of all ages are particularly susceptible to severe disease and death. General measures to improve hygiene are important but often difficult to implement because of their cost. An organized effort to promote careful handwashing with soap and water is the single most important control measure to decrease transmis sion rates in most settings. Common-source foodborne or waterborne outbreaks require prompt investigation and intervention whatever the infecting species. Institutional outbreaks may require special measures, including separate housing for cases and new admissions, a vigorous program of supervised handwashing, and repeated cultures of patients and attendants. The most difficult outbreaks to control are those that involve groups of young children (not yet toilet-trained) or the mentally decient, and those where there is an inadequate supply of water. Closure of affected day care centers may lead to placement of infected children in other centers with subsequent transmission in the latter, and is not by itself an effective control measure. Preventive measures: Same as those listed under typhoid fever, 9A1-9A10, except that no commercial vaccine is available. Control of patient, contacts and the immediate environment: 1) Report to local health authority: Case report obligatory in many countries, Class 2 (see Reporting). Recognition and report of outbreaks in child care centers and institutions are especially important. Because of the small infective dose, patients with known Shigella infections should not be employed to handle food or to provide child or patient care until 2 successive fecal samples or rectal swabs (collected 24 or more hours apart, but not sooner than 48 hours after discontinuance of antimicrobials) are found to be Shigella-free. Patients must be told of the importance and effectiveness of handwashing with soap and water after defecation as a means of curtailing transmission of Shigella. In communities with an adequate sewage disposal system, feces can be discharged directly into sewers without prelim inary disinfection. Thorough handwashing after defecation and before handling food or caring for children or patients is essential if such contacts are unavoidable. Cultures of contacts should generally be conned to food handlers, attendants and children in hospitals, and other situations where the spread of infection is particularly likely. Antibiotics, selected accord ing to the prevailing antimicrobial sensitivity pattern of where cases occur, shorten the duration and severity of illness and the duration of pathogen excretion. They should be used in individual cases if warranted by the severity of illness or to protect contacts. During the past 50 years Shigella have shown a propensity to acquire resistance against newly introduced antimicrobials that were initially highly effective. Multidrug resistance to most of the low-cost antibiotics (ampicillin, trimethoprim-sufamethox azole) is common and the choice of specic agents will depend on the antibiogram of the isolated strain or on local antimicrobial susceptibility patterns. In many areas, the high prevalence of Shigella resistance to trimethoprim-sufame thoxazole, ampicillin and tetracycline has resulted in a reliance on uoroquinolones such as ciprooxacin as rst line treatment, but resistance to these has also occurred. The use of antimotility agents such as loperamide is contraindi cated in children and generally discouraged in adults since these drugs may prolong illness. If administered in an attempt to alleviate the severe cramps that often accompany shigellosis, antimotility agents should be limited to 1 or at most 2 doses and never be given without concomitant antimicrobial therapy. Disaster implications: A potential problem where personal hygiene and environmental sanitation are decient (see Typhoid fever). Except for a laboratory-associated smallpox death at the University of Birmingham, England, in 1978, no further cases have been identied. Because of increasing concerns about the potential for deliberate use of clandestine supplies of variola virus, it is important that health care workers become familiar with the clinical and epidemiological features of smallpox and how it can be distinguished from chickenpox. Fatalities normally occurred between the fth and seventh day, occasionally as late as the second week. Fewer than 3% of variola major cases experienced a fulminant course, characterized by a severe prodrome, prostration, and bleeding into the skin and mucous membranes; such hemorrhagic cases were rapidly fatal. The rash of smallpox could also be signicantly modied in previously vaccinated persons, to the extent that only a few highly atypical lesions might be seen. In such cases, prodromal illness was not modied but the maturation of lesions was accelerated with crusting by the tenth day. Smallpox was most frequently confused with chickenpox, in which skin lesions commonly occur in successive crops with several stages of maturity at the same time. The chickenpox rash is more abundant on covered than on exposed parts of the body; the rash is centripetal rather than centrifugal. Smallpox was indicated by a clear-cut prodromal illness; by the more or less simultaneous appearance of all lesions when the fever broke; by the similarity of appearance of all lesions in a given area rather than successive crops; and by more deep-seated lesions, often involving sebaceous glands and scarring of the pitted lesions (chickenpox lesions are supercial and chickenpox rash is usually pruritic). Although the rash was like that in ordinary smallpox, patients generally experienced less severe systemic reactions, and hemorrhagic cases were virtually unknown. Laboratory conrmation used isolation of the virus on chorioallantoic membranes or tissue culture from the scrapings of lesions, from vesicular or pustular uid, from crusts, and sometimes from blood during the febrile prodrome. Electron microscopy or immunodiffusion technique often permitted a rapid provisional diagnosis. Because of the relatively long period of incubation for smallpox, vaccination within a 4-day period after exposure can prevent or attenuate clinical illness. Vaccination with licensed smallpox vaccine is recommended for all laboratory workers at high risk of contracting infection, such as those who directly handle cultures or animals contaminated or infected with vaccinia or other orthopoxviruses that infect humans. It may be consid ered for other health care personnel who are at lower risk of infection, such as doctors and nurses whose contact with these viruses is limited to contaminated dressings. Vaccination is contraindicated in persons with decient immune systems; persons with eczema or certain other dermatitis disorders; and pregnant women. Booster vaccinations are recommended within 10 years in categories for which vaccine is recom mended.
Order 5mg medex with mastercard. The Ebola Virus Explained — How Your Body Fights For Survival.
References
- Daneshmand S, Quek ML, Huffman JL. Endoscopic management of upper urinary tract transitional cell carcinoma: long-term experience. Cancer 2003;98(1):55-60.
- Hall JE: Guyton and Hall textbook of medical physiology, ed 12, Philadelphia, 2010, Saunders. 13.
- Costa C, Vendeira P: Does erectile tissue angioarchitecture modify with aging? An immunohistological and morphometric approach, J Sex Med 5(4):833n840, 2008.
- Estep T, Bucci E, Farmer M, et al: Basic science focus on blood substitutes: A summary of the NHLBI Division of Blood Diseases and Resources Working Group Workshop, March 1, 2006, Transfusion 48:776-782, 2008.
- Hagan KW, Braren V, Viner NA, et al: Extramammary Pagetis disease in the scrotal and inguinal areas, J Urol 114:154n156, 1975.
