Pristiq
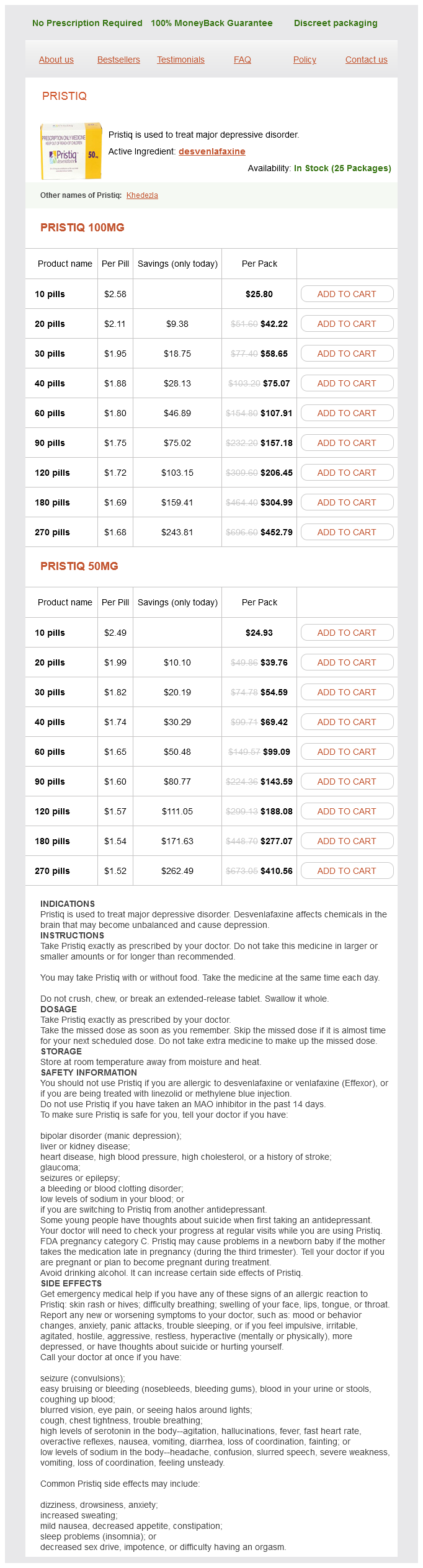
Yakoub Khalaf
- Guy? and St Thomas?Hospital Foundation Trust, Guy?
- Hospital, London
A comorbid dysthymic disorder thus appears to worsen the prognosis for major depression treatment 4s syndrome purchase 50 mg pristiq mastercard, by increasing the risk of either chronicity or recurrence medications images pristiq 100 mg overnight delivery. It should be noted that the diagnostic criteria for dysthymia have been modified over the years medications restless leg syndrome order pristiq 50 mg mastercard, making it difficult to interpret such findings accurately medications memory loss buy cheap pristiq 100 mg on-line. It is also believed (see Scott 1998) that experiencing a depression can bring about personality changes medicine for high blood pressure order pristiq 100 mg overnight delivery. The 28 persons who experienced their first-ever depressive episode during this six-year period were compared to 528 persons who had never had a depression symptoms enlarged prostate discount pristiq 100 mg with amex. Subjects who experienced a depression showed no personality changes after it, but they did have higher premorbid scores for introversion and emotional dependency. Life events and social support No evidence was found in the selected studies for any effects of recent life events as predictors of chronicity, but we should note that different instruments were used to assess life events. One study of depressed women in treatment (Brown et al, 1994) did link a chronic course of depression to adverse childhood experiences (sexual or physical abuse or neglect) and to current interpersonal problems. These findings were confirmed for lower-class depressed women in an identical study in the community (Brown & Moran, 1994). Because both studies used depressions of long duration as an exclusion criterion, depressive episodes of recent onset were overrepresented. Keitner et al (1992) found that poor family relations had an adverse effect on the duration of depression. Keller et al (1992, 1994a, b) identified being married as a risk factor, whereby relationship quality was a possible influence. A study of depressed older patients and 23 depressed patients under age 65, who were followed for two years until recovery occurred, found a strong association in the younger group between low social support and the duration of the depressive episodes (Alexopoulos et al, 1996). Here again, neither life events nor social support showed any relation to the outcomes. Some evidence does exist that familial loading for mood disorders elevates the risk of chronicity (Scott, 1998; Kendler et al, 1997). Scott et al (1992), in their study of 55 hospitalised depressed patients, found the duration of the preceding period without treatment to be the strongest predictor of chronicity. On the basis of their findings, the authors advise early intensive treatment to prevent chronicity. Coryell et al (1994) found, on the other hand, that the group who sought treatment had the longest duration of depression. Their explanation is that people seek treatment for depression only when it persists for a longer period of time. Discussion Most of the studies we selected to review are still subject to some criticism. Some of the research samples are quite small (Scott et al, 1992; Ormel et al, 1993) or are not fully representative of the patient population. These include the duration and the severity of depression, the number of previous depressive episodes, occurrence secondary to other conditions, and premorbid neuroticism. Comorbidity with somatic disorders, alcohol addiction, anxiety disorders and possibly dysthymia is also implicated. Whether life events have any influence is also unclear, and any links to social support or interpersonal problems needs to be confirmed in replication studies. Although the preponderance of studies carried out on hospitalised patients may very well have influenced our findings, we nevertheless come to the hypothesis that clinical features of the illness itself (duration, severity, previous episodes, comorbidity) gradually increase in importance during a long-term course of unipolar depression, whereas psychosocial factors play a major part during the early course of the illness. Other research has also suggested that psychosocial factors are mainly an issue in depressive episodes of brief duration (McLeod et al, 1992). On the basis of the studies that investigated effects of antidepressant treatments (Scott et al, 1992; Coryell et al, 1994), we conclude that prompt treatment at the onset of a depressive episode is urgently indicated for a substantial proportion of the depressed patients, especially for those who exhibit risk factors for chronicity. Any loss of time not only means 34 longer suffering for the patient but also appears to increase the risk of chronicity. The existing Dutch protocol for the treatment of depression (de Groot, 1995) can serve as a guideline. Many depressive episodes remit spontaneously; if this happens within a short time, then a strategy of watchful waiting seems justified for such patients. Effective recognition both of these patients and of the patients who will not recover spontaneously is therefore essential. This will require further research both in clinical populations and in the community. Such research will also need to verify whether the prompt initiation of treatment in patients with an increased risk of a chronic course of depression can indeed prevent their illness from becoming chronic. Rede uitgesproken bij de aanvaarding van de Leerstoel Sociale Psychiatrie aan de Faculteit der Medische Wetenschappen van de Rijksuniversiteit Groningen op dinsdag 1 april 1997. World Health Organization (1978) Mental Disorders: Glossary and Guide to their Classification in Accordance with the Ninth Revision of the International Classification of diseases. Nolen 1 De Gelderse Roos, Mental Health Care, Arnhem, the Netherlands 2 Netherlands Institute of Mental Health and Addiction, Utrecht, the Netherlands 3 University Medical Centre and Altrecht, Mental Health Care, Utrecht, the Netherlands Acta Psychiatrica Scandinavia 2000; 103:122-130 43 Summary Objective To investigate risk factors of poor one-year outcome of major depression in the general population and to compare the results with data from clinical populations. Younger age, severity of depression, longer duration of previous episodes, the presence of anhedonia and early awakening, external locus of control and multiple negative life events appear to be risk factors. Conclusion Poor outcome of major depression is frequent in the general population. Introduction In recent years attention has been focused on the poor outcome of depressive disorder in terms of relapse, recurrence or chronicity (1-3). Prospective studies on outcome of major depression have concentrated on relapse and recurrence (4-7), on chronicity (8-12) or either outcome (13, 14). In other studies (15, 16) no distinction between relapse, recurrence or chronicity was made. Several risk factors of poor outcome were identified and they can be categorised as follows: 1. Sociodemographic factors: lower socio-economic status was found a risk factor for chronicity (1, 10); older age is associated with an increased risk for relapse (4) but younger age for recurrence (5). Female sex was found a risk factor for recurrences (7) but not for chronicity (17, 18). Clinical factors: younger age of onset and greater severity of illness are risk factors for chronicity (1, 10, 15); longer length of depressive episodes for recurrences and chronicity (1, 7, 10) and higher number of previous episodes for relapses, recurrences and chronicity (1, 4-7, 10). Comorbidity with alcohol dependence was found a risk factor for chronicity (14), with somatic illnesses and anxiety disorders for poor outcome (15, 16), and with dysthymia (1, 4) for relapse, recurrence and chronicity. Personality characteristics: higher neuroticism is a risk factor for chronicity (9). Psychosocial factors: more negative childhood experiences and more ongoing difficulties were associated with chronicity (11). An influence from other negative life events on relapse or chronicity was not found (13) and the findings on social support on chronicity are contradictory (8, 12, 13). Treatment factors: length of period before antidepressant treatment was found a risk factor for chronicity (9). Undertreatment with antidepressants has been linked up with relapse, recurrence and chronicity (1) but in observational studies no causal relations between treatment and outcome can be made. Our conclusion from these studies is that risk factors for relapse, recurrence and chronicity do overlap but are probably not identical. Clinical factors appear to be the strongest predictors of poor outcome of depression (19). However, clinical populations (both inpatient and outpatient) were overrepresented in these studies in question. Our expectation is that in the general population psychosocial factors will have a stronger influence on the adverse outcome of major depression than in clinical populations. The analyses presented here are based on data from the first and second wave in 1996 and 1997. The first step of this large longitudinal study was to draw a sample of 90 Dutch municipalities. The stratification criteria were urbanicity (5 categories as classified by Statistics Netherlands) and adequate distribution over the 12 provinces. The number of households selected in each municipality was governed by the size of its population. The selected households were sent a letter of introduction signed by the Minister of Public Health requesting them to take part. Households with no telephone or with ex-directory numbers (18%) were visited in person. A respondent was randomly selected in each household, the member with the most recent birthday, on the condition that he or she was between 18 and 64 years of age and sufficiently fluent in Dutch to be interviewed. Persons who were not immediately available (owing to circumstances such as hospitalisation, travel or imprisonment) were contacted later in the year. If necessary the interviewers made a maximum of ten phone calls or visits to an address at different times and on different days. To optimise response and to compensate for possible seasonal influences, we spread the initial fieldwork over the entire period from February through December 1996. No adjustments had to be made to the procedure in the course of the fieldwork, and hence no supplemental respondents were drawn from specific social groups. We present data recorded at baseline (T0) in 1996 and at the first follow-up 12 months later (T1). Potential risk factors Independent variables assessed at baseline (T0) in the study were as follow: Sociodemographic factors. The comorbid disorders we deemed relevant were substance dependence, anxiety disorders, dysthymia and eating disorders. Comorbidity with somatic illnesses was assessed by means of a questionnaire listing 31 mostly chronic somatic conditions. Respondents were also asked whether they had received treatment for any of these conditions in the preceding 12 months. Neuroticism was assessed with the Groninger Neuroticism Questionnaire containing 14 items (28). Locus of control was assessed with the 5-item Mastery Scale (29), with high scores on mastery corresponding to an internal locus of control. In addition to the above-mentioned factors at T0 we evaluated several psychosocial factors measured at T1. It covered nine positive and nine negative life events and three ongoing difficulties in the period between T0 and T1. The life events were classified as changes in health status, changes in employment status, changes in relationship, changes in the family, changes in social contacts, traumatic experiences (all the above events being experienced by either the respondent or a significant other); changes in living conditions, expected changes in the future, and attainment or non-attainment of an important goal (events experienced by the respondent only). The sources of care included informal care (for instance physiotherapist/haptonomist, alternative care provider, self-help group), primary care, ambulatory mental health care and residential mental health care. Results Rate of poor outcome At T0, 305 persons met the criteria for a major depression in the preceding six months. In 10 cases 47 schizophrenia or bipolar disorder was diagnosed and those were excluded. Of those 160, 48 (30%) still had one or more other diagnoses at T1: eating disorder (1), dysthymic disorder (2), substance abuse or dependence (19) and anxiety disorder (36). In 43 of these cases this diagnosis had already been present at T0 as an comorbid diagnosis. In the total sample, attrition was only weakly associated with psychopathology at baseline, but not with depression (33). Risk factors Table 1 shows all potential risk factors of poor outcome with the outcomes of the bivariate analysis. Only two sociodemographic factors were found to be associated with poor outcome: female gender and unemployement. Amongst the clinical factors severity of depression, and especially depression with psychotic features, was strongly associated with poor outcome. At the symptomatic level, psychomotor agitation or retardation, anhedonia and early morning awakening showed significant relations to poor outcome. Comorbidity with dysthymia and with anxiety disorders did appear to constitute a higher risk. Comorbidity with eating disorders, substance dependence and somatic illnesses were not significantly related to an adverse course. Of the personality characteristics assessed, high neuroticism was found to be strongly associated with poor outcome and medium and high levels of mastery reduced the risk of a poor outcome almost equally. Both neuroticism and mastery were correlated with the severity of depression at baseline (neuroticism: Pearsons r = 0. Amongst the psychosocial factors, adverse childhood experiences were not found to be associated with a poor outcome, but the subjective experience of two or more negative life events and one or more ongoing difficulty between T0 and T1 was associated with an adverse course. Interestingly, the subjective experience of a medium level of social support but not a high level, was associated with a favourable effect on course. We next performed two multiple regression analyses on the variables found significant in the bivariate analysis, correcting for age and gender.
A pilot study of lithium carbonate plus divalproex sodium for the continuation and maintenance treatment of patients with bipolar I disorder treatment 001 - b purchase pristiq without a prescription. A double-blind comparison of lithium and chlorprom azine in the treatment of manic states medications ms treatment pristiq 50 mg line. Discontinuation of mainte nance treatment in bipolar disorder: risk and implications treatment cervical cancer order pristiq discount. Lamotrigine-induced car bamazepine toxicity: an interaction with carbamazepine-10 symptoms pinched nerve neck order cheap pristiq line, 11 epoxide treatment for depression buy discount pristiq online. In their original publication treatment statistics buy discount pristiq, Delay and co-workers (1952) described the benefits of chlorpromazine in five patients who were severely agitated, three of them suffering from psychotic mania. They suggested that antipsychotic agents were "life saving", as their use prevented the exhaustion and dehydration secondary to severe agitation. Antipsychotic agents therefore represent the oldest pharmacological treatment for acute mania, not only for those suffering from schizophrenia, but also those suffering from bipolar disorder. In the 1950s and 1960s chlorpromazine was instrumental in the treatment of the severely mentally ill. It is possible that many patients treated with antipsychotics at that time would be diagnosed as bipolar using modern criteria. In the 1970s, when lithium became available in the United States, the use of antipsychotics became a second option, primarily because of their adverse effect potential. In the late 1980s and early 1990s the use of the anticonvul sant divalproex sodium further relegated the use of antipsychotic agents. More recently, with the availability of new atypical antipsychotic agents, a renewed interest in antipsychotic agents has evolved in the field. This chapter will review the use of both typical and atypical antipsychotic agents in the treatment of acute mania. The only placebo controlled study of a typical antipsychotic agent was conducted by Klein (1967) in the 1960s. This study clearly demonstrated the efficacy of a conven tional antipsychotic in acute mania. The authors compared chlorpromazine (1200 mg/day) with imipramine (300 mg/day) and placebo in a 7-week study. The major finding was the superiority of chlorpromazine over both placebo and imipramine. A number of head-to-head comparisons between chlorpromazine and lithium were published in the 1970s. Most studies found no difference in terms of overall response and onset of response when chlorpromazine was compared to lithium (Tran et al. Specifically, patients who were randomized to lithium in a six-point severity scale improved 18% during the first week of treatment and 46% by week four. In comparison, patients randomized to chlorpromazine improved only 2% by the first week and 36% at week three. However, in those patients who were classified as mildly active the response to lithium appeared more robust. The investigators concluded that lithium appeared more effective in the improvement of affective symptoms, but that chlorpromazine was more effective in agitated patients. The popularity of haloperidol can be attributed to its fast onset of action, and its availability as a short-acting intramuscular and long-lasting depot formulations. Its short-acting intra muscular injection has a peak plasma concentration of 20 minutes. Having less anticholinergic side-effects than chlorpromazine, it has become a popu lar treatment in emergency rooms. The first study that compared haloperi dol with lithium was conducted by Garfinkel et al. Patients were randomized to haloperidol alone, lithium alone, or the combination of the two. After 8 days of treatment a significant improvement was observed with haloperidol alone, and with Antipsychotics in acute mania 375 haloperidol and lithium, but no improvement was observed in the patients treated with lithium. In addition, the combination of lithium and haloperidol did not appear to be superior to the use of haloperidol monotherapy. Importantly, the faster onset of action of haloperidol was seen specifically in the decrease of motor activity and agitation. However, by the end of the 3-week period the improvement noticed in patients receiving lithium was superior to those receiving haloperidol. An interesting study published by McElroy and colleagues (1996) com pared divalproex oral loading with haloperidol. The investigators studied 36 patients, of whom 21 were randomly assigned to divalproex oral loading 20 mg/kg per day, and 15 were randomized to haloperidol 0. The investigators found that divalproex oral loading and haloperidol were equally effective in improving manic symptoms. The findings of this study suggested that divalproex sodium was as effective as haloperidol, not only in terms of reductions in manic symptoms, but also of psychotic symptoms; with both drugs showing significant improvement after 3 days of treatment. The investigators concluded that divalproex sodium was as effective as haloperidol, but offered a more benign adverse effect profile. The investigators found that, by week one, 32% of patients randomized to haloperidol and 23% randomized to chlorpromazine showed significant improvement. Tohen penthixol and haloperidol found that the two drugs were equally effective in overall efficacy and action in acute mania (Baastrup et al. Primozide One of the most potent typical antipsychotic drugs, primozide, has also been studied in the treatment of acute mania. The authors concluded that the initial effects of chlorpromazine appeared to be related to sedative effects. In summary, typical antipsychotic agents have been used in the treatment of mania since they first appeared in the early 1950s. High-potency typical antipsychotics such as haloperidol or primozide appear to be more effective and have a faster onset of action than chlorpromazine. A major concern that remains regarding the use of typical antipsychotics is their adverse effect profile, including tardive dyskinesia, hyperprolactinaemia, and neuro leptic malignant syndrome. In addition, typical antipsychotics have been found to be depressogenic (Kukopulos et al. Considering their possible depressogenic effects, the use of typical anti psychotics in acute mania appears limited as they have only a unidirectional therapeutic effect. The latter is defined as an improvement of the symptoms of acute mania, but lack of improvement in the symptoms of depression or even worsening of depressive symptoms. This limitation has restricted the use of typical antipsychotic agents to the acute phase of the condition. It has been estimated that more than 85% of patients with acute mania receive a typical antipsychotic agent (Tohen et al. With the availability of the newer antipsychotic agents that provide a more benign adverse effect profile, and possibly mood-stabilizing proper Antipsychotics in acute mania 377 ties, there has been renewed interest in the use of antipsychotic agents in the treatment of acute mania. Some investigators have suggested that bipolar patients may have an increased risk of developing acute dystonia, akathisia, and tardive dyskine sia (Nasrallah et al. An additional risk associated with the typical antipsychotic agents is neuroleptic malignant syndrome. A possible association between affective disorders and tardive dyskinesia has been reviewed by a number of investigators. Kane and Smith (1982) found that the cumulative risk of developing tardive dyskinesia after being exposed to neuroleptics for at least 6 years was 26% for bipolar patients, compared to 18% for patients with schizophrenia. On the other hand, other investigators have not found a higher risk treating affective disorder patients. Specifically, Morgenstern and Glazer (1993), in a 5-year, follow-up study of close to 300 patients, found that psychiatric diagnosis was not a risk factor. In terms of severity of tardive dyskinesia, Glazer and Morgenstern (1988) discovered that patients with affective disorders had a more severe form of tardive dyskinesia. To summarize, although there is some literature suggesting that affective disorders may be a risk factor for developing tardive dyskinesia in patients exposed to typical antipsychotics, the findings are not compelling. Another consideration is to consider outcome as the severity of tardive dyskinesia rather than the relative risk of developing the condition. In this regard it is possible that patients with affective disorders who may develop tardive dyskinesia may be more incapacitated. Nonetheless, with the availability of other compounds such as lithium, anticonvulsants, or the atypical anti psychotic agents, the use of typical antipsychotics in affective disorders needs to be clearly justified. The superiority of the atypical agents also includes a more benign adverse effect profile with a lower risk of extrapyramidal side-effects, lower risk of tardive dyskinesia, lower risk of hyperprolactinaemia, and lower risk of anticholinergic side-effects. In addition to safety concerns the atypical agents appear to have a wider therapeutic spectrum in patients with schizo phrenia. Tohen agents, due to an affinity to serotonin and norepinephrine receptors, may have mood-altering properties. Clozapine Reports of the efficacy of clozapine in bipolar and schizoaffective disorder first appear in literature in the early 1970s (Faltus et al. A number of publications have found clozapine to be highly effective in the treatment of bipolar disorder. However, the vast majority of those studies have been case reports or open-label trials. The authors identified a limited number of controlled studies that included patients with psychotic mood disorders or schizoaffective disorders. Of note, a double-blind com parison study was recently published by Barbini et al. The authors concluded that patients receiving clozapine had a faster onset of action than those receiving chlorpromazine. The difference was statistically significant at the first assessment at week two, and remained significant at week three. The review included two double blind studies, eight open-label, 10 retrospective studies and 10 case reports. Of those 30 studies, 10 provided information that enabled the authors to estimate an overall assessment of the efficacy of clozapine in terms of the percentage of patients responding to clozapine (McElroy et al. Of those 10 studies a total of 350 patients with psychotic mood disorders were treated with clozapine; of which these patients had a bipolar disorder and 221 had a schizoaffective disorder in the bipolar phase of the illness. When those patients were compared with schizophrenic patients in seven of the 10 studies (n = 692), the response of the schizophrenic patients was 61. The first one, conducted by Calabrese and colleagues (1996), reported Antipsychotics in acute mania 379 the use of clozapine in 25 patients with acute mania, non-responsive to lithium, valproate, and typical antipsychotics. Criteria for non-response included the use of lithium carbonate at a blood level of 0. In addition, patients were required to have a history of not responding to a 6-week trial of a typical antipsychotic at a dose equivalent of 20 mg of haloperidol. The authors found that, in 22 of the 25 patients who completed the trial, 72% (18) had a marked improvement, and statistical significance was attained in the first week of treatment. A similar study, conducted at McLean Hospital (Tohen and Zarate 1998), included 24 patients who had a previous history of failing to respond to typical antipsychotics (chlorpromazine 500 mg or equivalent or lithium 0. Fifteen patients were able to complete this 13-week trial, of whom 87% were classified as very much or much improved. In the Young Mania Rating Scale a 50% improvement was achieved in 93% of the patients. The studies conducted by Calabrese and colleagues, and at McLean Hospital, suggest that clozapine may be effective in treatment-resistant manic patients. Although the efficacy of clozapine in acute mania appears convincing, less evidence is available for its effects as a mood stabilizer. After the patients were treated with clozapine the mean number of hospital izations was 0. In another report by Suppes and colleagues (1999), there was a significant improvement in psychotic and affective symptoms 6 months after being randomized through either clozapine or usual treatment. In a retrospective review that included 52 patients with bipolar disorder, 81 with schizoaffective disorder, and 14 with psychotic depression, the authors found that psychotic mania and schizoaffective bipolar patients had significantly better outcomes than patients with psychotic depression or schizoaffective-depressed type; suggesting that the index episode of mania or schizoaffective bipolar type predicted a better outcome. In addition, patients with a psychotic affective disorder had a better outcome in social 380 M. Tohen functioning compared to 40 patients with schizophrenia who were followed as a comparison group. A number of other case reports have also suggested that risperidone has mood-altering properties (Hillert et al. Similarly, Keck and colleagues (1995), in a retrospective chart review, found that patients with bipolar disorder or schizoaffective disorder depressed type had a good response when risperidone was added to mood stabilizers. The authors concluded that monotherapy with risperi done was of comparable efficacy to that of lithium and haloperidol. This review included 150 patients with psychotic disorders, including 47 patients with bipolar disorder with psychotic features, 29 patients with schizophrenia, 23 patients with schizoaffective disorder bipo lar type, 17 patients with schizoaffective disorder depressive type, 22 patients with major depression with psychotic features, and 12 patients with psychosis not otherwise specified. Of interest in this review is that Antipsychotics in acute mania 381 patients more likely to respond to olanzapine had a bipolar disorder diagno sis, were younger, female, and had a shorter duration of illness.
In addition medications 5113 buy cheap pristiq 100mg on line, such taper symptoms treatment hyperthyroidism cheap pristiq 50mg visa, side effects medicine pill identification order pristiq 50 mg without a prescription, adherence treatment plan goals and objectives buy pristiq 50 mg overnight delivery, and functional status ing can help minimize the incidence of antidepressant during this period of high vulnerability is strongly rec medication discontinuation syndromes medicine 100 years ago purchase pristiq from india, particularly with ommended medications kidney infection purchase online pristiq. If a patient does suffer a recurrence after dis paroxetine and venlafaxine (98, 163, 164). Discontinuation continuing medication, treatment should be promptly syndromes are problematic because their symptoms in reinitiated. Usually, the previous treatment regimen to clude disturbances of mood, energy, sleep, and appetite which the patient responded in the acute and continuation and can therefore be mistaken for or mask signs of relapse phases should be reinitiated (520). Consequently, patients should be advised not to currence following discontinuation of antidepressant stop medications abruptly and to take medications with therapy should be considered to have experienced another them when they travel or are away from home. Discontin major depressive disorder episode and should receive uation syndromes have been found to be more frequent af adequate acute-phase treatment followed by continua ter discontinuation of medications with shorter half-lives, tion-phase treatment and possibly maintenance-phase and patients maintained on short-acting agents should treatment. In patients at high risk for suicide creased mortality in the study subjects as a result of suicide and in whom a particularly rapid antidepressant response (531). In making decisions about treat permit removal of potentially dangerous items, such as ment, this awareness of a potential increase in suicidal weapons and personal belongings that could cause harm thinking and behavior in children, adolescents, and young. For adults age 65 years or older, a review behavior, co-occurring substance abuse, the availability of the evidence from clinical trials showed a decrease in and adequacy of social supports, and the nature of the the risk of suicidal thinking or behaviors with antidepres doctor-patient alliance. Many depressed patients members can also play an important role in detecting and report slowed thoughts, poor concentration, distractibility, preventing suicidal behaviors. They also dis tient, the psychiatrist should educate those close to the play diminished attention to self-care and to their environ patient concerning appropriate interventions and encour ment. For Although information on such risk continues to evolve, a individuals who exhibit symptoms of a dementia syndrome, predictive relationship to suicide has never been demon it is crucial that any underlying depressive disorder be iden strated. More ible causes (such as vitamin B12 deficiency, folate deficiency, recently, meta-analyses of data from clinical trials have testosterone deficiency, substance use). The latter, especially in more ad terms, it is estimated that one to three of 100 individuals vanced stages, typically do not recognize their cognitive age 25 years or younger could potentially have an increase failures, since insight is impaired. In contrast, depressed in suicidal thoughts or behaviors with antidepressant patients may report being unable to think or remember. Practice Guideline for the Treatment of Patients With Major Depressive Disorder, Third Edition 61 dysfunction lack the signs of cortical dysfunction. Nevertheless, distinguishing extreme negativism; peculiarities of voluntary movement, dementia from depression-related cognitive dysfunction as evidenced by posturing, stereotyped movements, man can be difficult, particularly as the two may coexist. For fur nerisms, or grimacing; and echolalia or echopraxia (556, ther discussion of the co-occurrence of dementia and de 557). Catatonic signs often cognitive dysfunction alerts the psychiatrist to the need dominate the clinical presentation and may be so severe as for treatment of the underlying major depressive disorder, to be life-threatening, compelling the consideration of ur which should in turn reduce the signs and symptoms of gent somatic treatment. Intravenous administra tain types of executive cognitive dysfunction predict greater tion of a benzodiazepine. After catatonic manifestations recede, antidepres incongruent with the depressed mood. Recognition of sant medication treatments may be needed during acute psychosis is essential among patients with major depres and maintenance phases of treatment. Pa current psychosis and hence indicate the need for mainte tients with catatonia may have an increased susceptibility nance treatment. Pharmacotherapy can also be used as a first-line Melancholic features describe characteristic somatic treatment option for major depressive disorder with psy symptoms, such as the loss of interest or pleasure in all, or chotic features. Psychotic depression typically responds almost all, activities or a lack of reactivity to usually plea better to the combination of an antipsychotic and an an surable stimuli. Psychotherapy may be less appropriate for patients with melancholia (563), particularly if the symptoms pre b. As a primary treatment, light Major depressive disorder with atypical features is charac therapy may be recommended as a 1 to 2-week time-limited terized by a pattern of marked mood reactivity and at least trial (395), primarily for outpatients with clear seasonal two additional symptoms, including leaden paralysis, a patterns. For patients with more severe forms of major long-standing pattern of interpersonal rejection sensitivity, depressive disorder with seasonal pattern, the use of light significant weight gain or increase in appetite, and hyper therapy is considered adjunctive to pharmacological in somnia (the latter two of which are considered reversed tervention. Co-occurring psychiatric disorders ated with an earlier age at onset of depression and a greater Co-occurring psychiatric disorders generally complicate degree of associated anxiety disorders, and frequently have a more chronic, less episodic course, with only partial in treatment. Electroconvulsive therapy is also effective in treat underlying major depressive disorder. Dysthymic disorder severity of specific symptoms as well as safety consider ations should help guide the choice of treatment for major Dysthymic disorder is a chronic mood disorder with depressive disorder with atypical features. For example, if symptoms that fall below the threshold for major depres a patient does not wish to , cannot, or appears unlikely to sive disorder. Because of this, it may escape notice and adhere to the dietary and medication precautions associ may be inadequately treated. Unfortunately, clinical symptoms, which is not the result of seasonally related trials provide little evidence of the relative efficacies of psychosocial stressors. The most common presentation of dysthymic disorder resembles that for episodes of in the northern hemisphere is the regular appearance of major depressive disorder; responses to antidepressant symptoms between early October and late November and medications by patients with dysthymic and chronic regular remission from mid-February to mid-April. Epi major depressive disorders have been comparable to the sodes of major depressive disorder with seasonal pattern responses by patients with major depressive disorder frequently have atypical features such as hypersomnia and episodes (580). Some of these patients experience manic or medication can reverse not only the acute major depres hypomanic episodes as well; hence, it is important to di sive episode but also the co-occurring dysthymic disorder agnose bipolar disorder when appropriate. Practice Guideline for the Treatment of Patients With Major Depressive Disorder, Third Edition 63 Patients with dysthymic disorder, as well as patients sessive-compulsive disorder may appear as a co-occurring with chronic and severe major depressive disorder, typi condition in some patients with major depressive disor cally have a better response to the combination of phar der. Anxiety disorders the psychiatrist should therefore screen for depression in As a group, anxiety disorders are the most commonly oc this population, although this is sometimes challenging curring psychiatric disorders in patients with major de (539). A 2005 epidemiological study sion in Dementia, which incorporates self-report with found that among individuals with major depressive dis caregiver and clinician ratings of depressive symptoms order, 62% also met the criteria for generalized anxiety (596). Antidepressants are likely to be efficacious in panic attacks, are frequent co-occurring symptoms of treatment of depressive symptoms, but they do not im major depressive disorder. Individuals larly when accompanied by racing or ruminative thoughts, with dementia are particularly susceptible to the adverse should alert the clinician to the possibility of a mixed effects of muscarinic blockade on memory and attention. Therefore, individuals with dementia generally do best In studies of major depressive disorder with a co when given antidepressant medications with the lowest occurring anxiety disorder, both depressive symptoms and possible degree of anticholinergic effect. Alternatively, worsen rather than alleviate anxiety symptoms, including some patients do well when given stimulants in small panic attacks; patients should be so advised, and these doses. Electroconvulsive therapy is also effective in major medications should be introduced at low doses and slowly depressive disorder superimposed on dementia. Adjunctive anti be used if medications are associated with an excessive risk panic agents, such as benzodiazepines, may be necessary of adverse effects, are not tolerated, or if immediate reso as well. Because benzodiazepines (539) contains more information about the treatment of are not antidepressants and carry their own adverse effects depression and dementia. Substance use disorders for patients with major depressive disorder who have co Major depressive disorder frequently occurs with alcohol occurring anxiety symptoms. Therefore, the adjunctively with other antidepressive treatments, how psychiatrist should obtain a detailed history of the pa ever (591). If the evaluation reveals a substance use Obsessive-compulsive symptoms are also common in disorder, this should be addressed in treatment. In addition, ob with major depressive disorder who has a co-occurring Copyright 2010, American Psychiatric Association. Patients with virtually any personality dis Detoxifying patients before initiating antidepressant order exhibit a less satisfactory antidepressant medication medication therapy is advisable when possible (110). An treatment response, in terms of both social functioning tidepressants may be used to treat depressive symptoms and residual major depressive disorder symptoms, than do following initiation of abstinence if symptoms do not im individuals without personality disorders (616). It is difficult to identify patients who should ity disorders tend to interfere with treatment adherence begin a regimen of antidepressant medication therapy and development of a psychotherapeutic relationship. Fur soon after initiation of abstinence, because depressive thermore, many personality disorders increase the risk of symptoms may have been induced by intoxication and/or episodes and increase time to remission of major depres withdrawal of the substance. Patients with various personality pressive disorder, a history of major depressive disorder disorders also showed high rates of new-onset major de preceding alcohol or other substance abuse, or a history of pressive episodes in a large prospective study (619) and were major depressive disorder during periods of sobriety raises at higher risk of attempting suicide than patients without the likelihood that the patient might benefit from antide a co-occurring personality disorder (620). Comparing the temporal pattern of symptoms major depressive episode, as depressive symptoms may ex with the periods of use and abstinence of the substance aggerate or mimic personality traits. Repeated, lon pressive disorder for these patients can cause the apparent gitudinal psychiatric assessments may be necessary to dis personality disorder symptoms to remit or greatly dimin tinguish substance-induced depressive disorder from co ish. Depressed patients may believe that their current occurring major depressive disorder, particularly because symptoms have been present from early life, when in fact some individuals with substance use disorders reduce they only began with the current episode. Such misper their substance consumption once they achieve remission ceptions often hinder accurate diagnosis. Personality disorders line personality disorder, the personality disorder must For patients who exhibit symptoms of both major depres also be addressed in treatment. Major havioral impulsivity and dyscontrol can also be treated Copyright 2010, American Psychiatric Association. Practice Guideline for the Treatment of Patients With Major Depressive Disorder, Third Edition 65 with low-dose antipsychotics, lithium, and some antiepi important relationship or life role. Monoamine oxidase inhibitors, al true in initial episodes of depression, with psychosocial though efficacious, are not recommended due to the risk of stressors being less associated with the onset of recurrent serious side effects and the difficulties with adherence to episodes (632). Eating disorders are also common in patients with major Ambivalent, abusive, rejecting, or highly dependent family depressive disorder (631). Selective serotonin reuptake relationships may predispose an individual to major depres inhibitors are the best studied medications for treatment sive disorder. The psychiatrist should screen for such fac of eating disorders, with fluoxetine having the most evi tors and consider family therapy, as indicated, for these dence for the effective treatment of bulimia nervosa (170). Family therapy may be conducted in conjunction Antidepressants may be less effective in patients who are with individual and pharmacological therapies. Even for in severely underweight or malnourished, and normalizing stances in which there is no apparent family dysfunction, it weight should take priority in these patients. Patients with chronic anorexia the psychiatrist may choose to treat a major depressive nervosa have in general been less responsive to formal episode with an antidepressant, even if a major stressor psychotherapy. Electroconvulsive therapy has not generally been major depressive disorder suggests the potential utility of useful in treating eating disorder symptoms. Although a psychotherapeutic intervention coupled, as indicated, there are few data to guide treatment of co-occurring ma with somatic treatment. However, grief, the natural Practice Guideline for the Treatment of Patients With Eating response to bereavement, resembles depression, and this Disorders, Third Edition (170). Psychiatrists treating be reaved individuals should differentiate symptoms of normal B. Major psychosocial stressors and psychoeducation about symptoms and the course of Major depressive disorder may follow a substantial ad mourning; complicated grief requires a targeted psycho verse life event, especially one that involves the loss of an therapy, with or without concomitant medication (535, Copyright 2010, American Psychiatric Association. Acute grief is the universal reaction to loss of a loved Specific cultural variables may also influence the assess one, and it is a highly dysphoric and disruptive state (641). For exam Acute grief is characterized by prominent yearning and ple, in some cultures, depressive symptoms may be more longing for the person who died, recurrent pangs of sad likely to be attributed to physical diseases (658). In addi ness and other painful emotions, preoccupation with tion, language barriers can impede accurate psychiatric thoughts and memories of the person who died, and rela diagnosis and effective treatment (659), and, even when tive lack of interest in other activities and people. Despite speaking the same language, individuals of different cul the similarity with depression, only about 20% of be tures may use different psychological terms to describe reaved people meet the criteria for major depressive dis their symptoms (6, 7). Successful mourning leads to resolution of acute dividual experience should not be underestimated in the grief over a period of about 6 months. The assessment and treat mains as a permanent state in which there is ongoing sad ment process can also be influenced by religious beliefs ness about the loss often accompanied by ongoing feelings (5). Individuals with high levels of religious involvement of yearning for the person who died. However, when the may have diminished rates of major depressive disorder death is accepted, and grief integrated, the person is again (661, 662). Differences in the utilization of psychiatric services by Complicated grief is a recently recognized syndrome in some cultural and ethnic groups have been well docu which symptoms of acute grief are prolonged, associated mented.
Pristiq 50 mg overnight delivery. How Long Does it Take to Recover Alcohol Withdrawal Symptoms | शराब छोड़ने के लक्षण कब ठीक होते है |.
Instead treatment 7 february discount 100mg pristiq otc, major concepts or principles will be discussed not only in 0-8493-1492-5/03/$0 treatment zone guiseley purchase generic pristiq canada. It is clear that synovial joints are by far the most complex and sophisticated tribological systems that exist treatment kennel cough cheap 50 mg pristiq otc. We shall see that although numerous theories have been put forth to attempt to explain joint lubrication treatment abbreviation discount pristiq online, the mech anisms involved are still far from being understood walmart 9 medications order cheapest pristiq and pristiq. And when one begins to examine possible connec tions between tribology and degenerative joint disease or osteoarthritis medications zanaflex purchase 100mg pristiq overnight delivery, the picture is even more complex and controversial. Finally, this article does not treat the (1) tribological behavior of arti cial joints or partial joint replacements, (2) the possible use of elastic or poroplastic materials as arti cial cartilage, and (3) new developments in cartilage repair using transplanted chondrocytes. These are separate topics, which would require detailed discussion and additional space. Tribological processes are involved whenever one solid slides or rolls against another, as in bearings, cams, gears, piston rings and cylinders, machining and metalworking, grinding, rock drilling, sliding electrical contacts, frictional welding, brakes, the striking of a match, music from a cello, articulation of human synovial joints. Tribology is a multidisciplinary subject involving at least the areas of materials science, solid and surface mechanics, surface science and chemistry, rheology, engineering, mathematics, and even biology and bio chemistry. Although tribology is still an emerging science, interest in the phenomena of friction, wear, and lubrication is an ancient one. But there are some important basic principles needed to understand any study of lubrication and wear and even more so in a study of biotribology or biological lubrication phenomena. The problem was often treated strictly from a mechanical viewpoint, with little or no regard for the environment, surface lms, or chemistry. In the rst place, friction may be de ned as the tangential resistance that is offered to the sliding of one solid body over another. Friction is the result of many factors and cannot be treated as something as singular as density or even viscosity. Postulated sources of friction have included (1) the lifting of one asperity over another (increase in potential energy), (2) the interlocking of asperities followed by shear, (3) interlocking followed by plastic deformation or plowing, (4) adhesion followed by shear, (5) elastic hysteresis and waves of deformation, (6) adhesion or interlocking followed by tensile failure, (7) intermolecular attraction, (8) electrostatic effects, and (9) viscous drag. It is emphasized that friction is a force and not a property of a solid material or lubricant. Wear and Surface Damage One de nition of wear in a tribological sense is that it is the progressive loss of substance from the operating surface of a body as a result of relative motion at the surface. In comparison with friction, very little theoretical work has been done on the extremely important area of wear and surface damage. This is not too surprising in view of the complexity of wear and how little is known of the mechanisms by which it can occur. Variations in wear can be, and often are, enormous compared with variations in friction. For example, Joint Lubrication 75 practically all the coef cients of sliding friction for diverse dry or lubricated systems fall within a relatively narrow range of 0. Reduction of friction by a factor of two through changes in design, materials, or lubricant would be a reasonable, although not always attainable, goal. On the other hand, it is not uncommon for wear rates to vary by a factor of 100, 1000, or even more. A fth, fretting wear and fretting corrosion, combines elements of more than one mechanism. For complex biological materials such as articular cartilage, most likely other mechanisms are involved. The idea that friction causes wear and therefore, low friction means low wear, is a common mistake. Since friction and wear do not necessarily correlate with each other, the use of the word and in place of and/or in the above de nition is a common mistake to be avoided. The primary function of a lubricant is to reduce friction or wear or both between moving surfaces in contact with each other. They include automotive engine oils, wheel bearing greases, transmission uids, electrical contact lubricants, rolling oils, cutting uids, preservative oils, gear oils, jet fuels, instrument oils, turbine oils, textile lubricants, machine oils, jet engine lubricants, air, water, molten glass, liquid metals, oxide lms, talcum powder, graphite, molybdenum disul de, waxes, soaps, polymers, and the synovial uid in human joints. Almost any substance under carefully selected or special conditions can be shown to reduce friction or wear in a particular test, but that does not mean these substances are lubricants. This is an extremely important principle which applies to nonlubricated (dry) as well as lubricated systems. An additive may reduce friction and increase wear, reduce wear and increase friction, reduce both, or increase both. Although the reasons are not fully understood, this is an experimental observation. The effective or active lubricating lm in a particular system may or may not consist of the original or bulk lubricant phase. In a broad sense, it may be considered that the main function of a lubricant is to keep the surfaces apart so that interaction. The following regimes or types of lubrication may be considered in the order of increasing severity or decreasing lubricant lm thickness (Fig. Transition from hydrodynamic and elastohydrodynamic lubrication to boundary lubrication 4. A fth regime, sometimes referred to as dry or unlubricated, may also be considered as an extreme or limit. In addition, there is another form of lubrication that does not require relative movement of the bodies either parallel or perpendicular to the surface, i. Hydrodynamic Lubrication Theories In hydrodynamic lubrication, the load is supported by the pressure developed due to relative motion and the geometry of the system. In the regime of hydrodynamic or uid lm lubrication, there is no contact between the solids. The lm thickness is governed by the bulk physical properties of the lubricants, the most important being viscosity; friction arises purely from shearing of viscous lubricant. Contributions to our knowledge of hydrodynamic lubrication, with special focus on journal bearings, have been made by numerous investigators including Reynolds. The classic Reynolds treatment consid ered the equilibrium of a uid element and the pressure and shear forces on this element. Velocity distributions due to relative motion and pressure buildup were developed and added together. The solution of the basic Reynolds equation for a particular bearing con guration results in a pressure distribution throughout the lm as a function of viscosity, lm shape, and velocity. The total load W and frictional (viscous) drag F can be calculated from this information. The dimensionless term (U/W) is sometimes referred to as the hydrodynamic factor. It can be seen that doubling either the viscosity or velocity doubles the lm thickness, and that doubling the applied load halves the lm thickness. This regime of lubrication is sometimes referred to as the rigid isoviscous Joint Lubrication 77 or classical Martin condition, since the solid bodies are assumed to be perfectly rigid (non-deformable), and the uid is assumed to have a constant viscosity. At high loads with systems such as gears, ball bearings, and other high-contact-stress geometries, two additional factors have been considered in further developments of the hydrodynamic theory of lubri cation. One of these is that the surfaces deform elastically; this leads to a localized change in geometry more favorable to lubrication. The second is that the lubricant becomes more viscous under the high pressure existing in the contact zone, according to relationships such as: exp p p (4. In this concept, the lubricant pressures existing in the contact zone approximate those of dry contact Hertzian stress. It may also be described as the elastic-viscous type or mode of lubrication, since elastic deformation exists and the uid viscosity is considerably greater due to the pressure effect. In examining the elastohydro dynamic lm thickness equations, it can be seen that the velocity U is an important factor (h U 0. These studies may lead to a better understanding of not only lubricant lm formation in high contact-stress systems but lubricant lm failure as well. Two other possible types of hydrodynamic lubrication, rigid-viscous and elastic-isoviscous, complete the matrix of four, considering the two factors of elastic deformation and pressure-viscosity effects. In addition, squeeze lm lubrication can occur when surfaces approach one another. For more information on hydrodynamic and elastohydrodynamic lubrication, see Cameron [3] and Dowson and Higginson [4]. Transition from Hydrodynamic to Boundary Lubrication Although prevention of contact is probably the most important function of a lubricant, there is still much to be learned about the transition from hydrodynamic and elastohydrodynamic lubrication to 78 Biomechanics: Principles and Applications boundary lubrication. Several examples of experimental approaches to thin lm lubrication have been reported [3]. It is important in examining these techniques to make the distinction between methods that are used to determine lubricant lm thickness under hydrodynamic or elastohydrodynamic conditions. As we will see later, most experimental studies of synovial joint lubrication have focused on friction measurements, using the information to determine the lubrication regime involved; this approach can be misleading. Boundary Lubrication Although there is no generally accepted de nition of boundary lubrication, it is often described as a condition of lubrication in which the friction and wear between two surfaces in relative motion are determined by the surface properties of the solids and the chemical nature of the lubricant rather than its viscosity. This opens the door to the inclusion of elastohydrodynamic effects which depend in part on the in uence of pressure on viscosity. Increased friction under these circumstances could be attributed to increased viscous drag rather than solid-solid contact. According to another common de nition, boundary lubrication occurs or exists when the surfaces of the bearing solids are separated by lms of molecular thickness. Although a considerable amount of research has been done on this topic, an understanding of the basic mechanisms and processes involved is by no means complete. In many practical systems, the occurrence of the boundary lubrication regime is unavoid able or at least quite common. More particularly, the surface chemistry and interactions occurring with and on the solid surfaces are important. This includes factors such as physisorption, chemisorption, intermolecular forces, surface chemical reactions, and the nature, struc ture, and properties of thin lms on solid surfaces. It also includes many other effects brought on by the process of moving one solid over another, such as: (1) changes in topography and the area of contact, (2) high surface temperatures, (3) the generation of fresh reactive metal surfaces by the removal of oxide and other layers, (4) catalysis, (5) the generation of electrical charges, and (6) the emission of charged particles such as electrons. In examining the action of boundary lubricant compounds in reducing friction or wear or both between solids in sliding contact, it may be helpful to consider at least the following ve modes of lm formation on or protection of surfaces: (1) physisorption, (2) chemisorption, (3) chemical reactions with the solid surface, (4) chemical reactions on the solid surface, and (5) mere interposition of a solid or other material. The bene cial and harmful effects of minor changes in chemistry of the environment. Thus, the surface and chemical properties of the solid materials used in tribological applications become especially important. General Comments on Tribological Processes It is important to recognize that friction and wear depend upon four major factors, i. Readers are cautioned against the use of various terms in tribology which are either vaguely de ned or not de ned at all. We will see several examples of this common error in the discussion of joint lubrication research. The bones are covered by a thin layer of articular cartilage bathed in synovial uid con ned by synovial membrane. Basically, it consists of water (approximately 75%) enmeshed in a network of collagen bers and proteoglycans with high molecular weight. Articular cartilage also has no blood supply, no nerves, and very few cells (chondrocytes). Synovial uid functions as a joint lubricant, nutrient for cartilage, and carrier for waste products.
References
- Meyers MA, Oliphant M: Ascending retrocecal appendicitis. Radiology 1974; 110:295-299.
- Keeri-Szanto M: The subclavian vein, a constant and convenient intravenous injection site. AMA Arch Surg 72:179-181, 1956.
- Wilson W, van Donkelaar CC, van Rietbergen B, Huiskes R. A fibrilreinforced poroviscoelastic swelling model for articular cartilage. J Biomech 2005; 38(6):1195-204.
- Brown KT, Koh BY, Brody LA, et al. Particle embolization of hepatic neuroendocrine metastases for control of pain and hormonal symptoms. J Vasc Interv Radiol 1999;10(4):397-403.
- Moncada S, Gryglewski R, Bunting S, Vane JR. An enzyme isolated from arteries transforms prostaglandin endoperoxides to an unstable substance that inhibits platelet aggregation. Nature. 1976;263:663-665.
