Zetia

Thomas C. Gerber, MD, PhD
- Professor of Medicine and Radiology
- Mayo Clinic College of Medicine
- Rochester, Minnesota
- Consultant in Cardiology
- Mayo Clinic
- Jacksonville, Florida
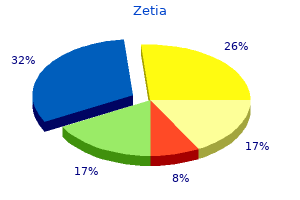
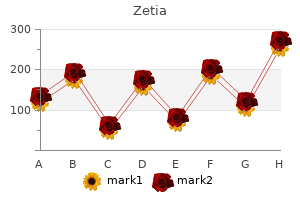
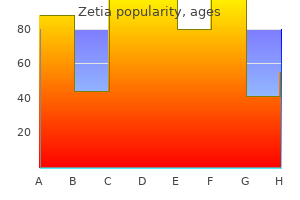
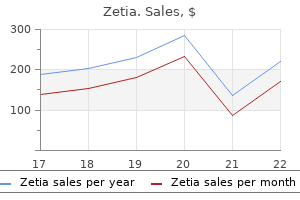
Additionally cholesterol lowering foods diet plan purchase zetia from india, some infants may have low cardiac output due to alterations following ligation (post ligation syndrome) cholesterol ratio desirable zetia 10 mg amex. Characterized by a repeating sequence (>=3) of prolonged pauses (>=3s) in breathing with periods of normal respiration (<20s) cholesterol lowering foods list pdf buy genuine zetia on-line. While commonly seen in nearly all infants cholesterol synthesis definition buy zetia pills in toronto, careful clinical assessment to rule out true apnea is necessary cholesterol ratio calculator buy generic zetia 10 mg on line. Xanthines such as caffeine lowering cholesterol triglycerides diet 10 mg zetia otc, aminophylline and theophylline are central stimulants that may improve diaphragmatic contraction and inhibit hypoxia-induced ventilation. Physiologic anemia of prematurity is often long-term and not necessarily pathologic. Neonatal red cells have short life spans and stressed marrow may exacerbate anemia. Further subclassification of severity is based on gestational age and chronologic age. Postnatal factors are related to immaturity such as ventilator associated injury (oxygen toxicity, barotrauma/volutrama, atelectasis), sepsis, pulmonary infection and poor nutrition. Later, the film may show pulmonary edema, airway cuffing, atelectasis, cystic changes, and air trapping. Enhancement of growth of normal lung tissue is accomplished in the absence of a ventilator and excess oxygen. Again, lung protective therapies such as avoidance of infection, ventilation and hyperoxia, as well as ensuring good nutrition are critical to long-term growth. They also have impaired growth due to increased caloric needs and may need to be on increased calorie formulas. Since lung parenchyma continues to grow until age eight, symptoms usually abate with time. Another indication for corticosteroid therapy is to supplement the corticosteroid insufficient infant. Courses have currently trended to 3 day bursts with a steroid-free period between bursts. It has a more physiologic half-life and agent is eliminated from body within 24hrs of dosing. This agent has been utilized in both treating the steroid deficient infant and supplementing the stressed premature infant. The hemorrhage may extend either into the ventricular space and/or the surrounding parenchyma of the lateral ventricle. The germinal matrix is adjacent to lateral ventricles and the site of neuronal and glial cell production and subsequent migration; it is a highly vascular area that involutes by 36 weeks gestation. Head ultrasound is the main diagnostic modality and classification is based on this modality of detection. Subarachnoid hemorrhages or secondary parenchymal injuries may be difficult to detect. It is also the most common cause of neurologic deficit and cerebral palsy in at risk infants. It is characterized by focal cystic necrotic lesions deep in the cerebral white matter. These may be seen at any time after birth, but generally appear between 2 and 4 weeks. It is the major cause of cognitive defects and impaired neurodevelopment in this population. In severe forms, retinal scarring, traction folds, and detachments can lead to blindness. In addition, selected infants born at >32 weeks gestational age deemed at risk (complicated clinical course). Infants are screened when they are 4-6 weeks chronological age, or 31-33 weeks postconceptual age. Retinal Zones Zone 1: Vessels extend less than twice the distance between the disc and macula. Weaning to Open Crib Generally thermal competence is achieved between 1500 to 2000 grams. Fever An infrequent sign of sepsis Less than 10% of febrile infants have culture-proven sepsis. However because of the potential toxicity of bilirubin, it is important to recognize hyperbilirubinemia and be aware of the risk factors for it. One third of healthy breast-fed infants have persistent jaundice beyond 2 weeks of age. The goal is to reduce the incidence of severe hyperbilirubinemia as well as acute bilirubin encephalopathy (the clinical central nervous system findings associated with bilirubin toxicity) and the more chronic kernicterus while minimizing harm such as increased parental anxiety, decreased breastfeeding and unnecessary costs and treatments. Increasing the frequency of nursing may decrease the likelihood of hyperbilirubinemia in breastfed infants. Jaundice should be assessed whenever vital signs are checked but at least every 8-12 hours. Jaundice is usually seen in the face first and progresses caudally, but visual estimation can lead to errors. A serum or transcutaneous bilirubin level should be checked in every infant who is jaundiced within the first 24 hours of life, or if there is any doubt about the degree of jaundice in any infant. The cause of jaundice should be investigated in any infant receiving phototherapy or if the level is rising rapidly (crossing percentiles on the nomogram). Infants with an elevated direct reacting bilirubin (conjugated) should have a urinalysis and urine culture. Sick infants or those jaundiced beyond 3 weeks should have a total and direct bilirubin level checked to identify cholestasis. Results of the newborn screen should be checked for thyroid abnormalities and galactosemia. There should be a demonstration of a decrease in total bilirubin concentration after 4-6 hours of phototherapy. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Any infant who is jaundiced and manifests signs of the intermediate or advanced signs of bilirubin encephalopathy should have immediate exchange transfusion. Recognize that the preparation time required for a double-volume exchange transfusion (often 4-6 hours). It is prudent to send blood for typing and cross-matching to the Blood Bank as soon as it is recognized that an exchange is possible. Dialogue with the Blood Bank may be essential for proper composition of the whole blood required for the procedure. It is also an option to temporarily interrupt breastfeeding and substitute formula. Supplementing the breastfed infant receiving phototherapy with expressed breast milk or formula if intake is inadequate, the weight loss is excessive or the infant seems dehydrated. These tend to be second-line agents and are used primarily in conjunction with a neurology consult. These injuries may often be independent of any symptoms during labor or delivery period. In fact, some of these injuries occur antenatally or may result of specific conditions or abnormal anatomy. This should occur at about 6 months of age and then subsequent evaluations as dictated by the specialist. The clinical presentation can vary widely from asymptomatic and an incidental finding to infants presenting with seizures to , extremely rarely, an infant with a catastrophic deterioration. Small bleeds are common in vaginal deliveries, but for a larger one or if symptomatic, evaluation is indicated. Work-up of coagulopathies and confirmation of vitamin K administration should be done in the symptomatic cases. Infants presenting in catastrophic demise and survive tend to have neurologic sequelae in follow-up. It can occur as a complication of lung diseases that cause respiratory failure in the newborn. These include perinatal aspiration syndrome, pneumonia or respiratory distress syndrome. Meconium aspiration syndrome: Meconium causes mechanical obstruction to the airways >resulting in air trapping, hyperinflation, ^ risk for pneumothorax, inactivation of surfactant, release of vasoconstrictors. Chemical pneumonitis leads to release of cytokines and leukotrienes that can increase pulmonary vasoconstriction. They also cause loss of surfactant function and decreased aeration of lungs and induce pulmonary edema by increasing vascular permeability. These changes consist of abnormal thickening of media and adventitia of pulmonary arteries and hypoxemia in the absence of recognizable parenchymal lung disease. Active precordium and systolic murmur of tricuspid insufficiency may be appreciated on cardiac exam. Although these criteria are still useful, certain caveats have to be considered to avoid errors in diagnosis. However, 2-site sampling for arterial blood is invasive and is not recommended for diagnosis. Monitoring preand post-ductal saturations is useful in gauging the response to pulmonary vasodilator therapy. It is important to consider the lungs and heart as one unit, connected by pulmonary circulation. Ideal management will involve optimizing lung expansion and cardiac output while achieving pulmonary vasodilation and maintaining systemic pressure. It is important to avoid excessive levels of 457 oxygen or ventilator pressures that can injure the lung. Hyperventilation can also have adverse effects on cerebral perfusion and induces hearing loss (blood supply to cochlea is part of cerebral circulation). Iloprost is the preferred agent since it can be given by intermittent nebulization, every 26 hours, depending on the duration of response. Milrinone works synergistically with inhaled prostacyclin in the same signaling axis. However, in this summary, Heart Rate and contractility are properties intrinsic to the heart itself and will be discussed. Mechanically, tachyarrhythmia can be classified as 1) reentry, 2) automaticity, 3) triggered activity. Reentry occurs when there are differential rates of conduction and is 462 triggered by a premature beat. Automaticity is a function of phase and depolarization ectopic activity, action potential. Slow rates (bradycardia) can be from the atrium (sinus bradycardia) or the ventricle. Other causes include sinus disease (post-operative) hypercalcemia hpyermagnesemia. Treatment includes identifying the cacuse if one is present, epinephrine, atropine, or pacemaker, Ventricular bradycardia are functional blocks, stable patients are treated with epinephrine, unstable patients are paced. Fast rates (tachycardia) can stem from the atrium or the ventricle and may be hemodynamically problematic or not. Atrial Muttler (saw tooth pattern rate 150) should get a trial of procainamide, digoxin or ibutalide (0. In acute decompensated heart failure, there are no medications that are associated with increased survival. Theoretically, the end point of therapy is to achieve a great stroke volume for the same or lower preload. There is a current study on whether hypothermia is helpful in the pediatric patient. If epinephrine is given endotracheally, and is given in an acidic carrier, the indicator may turn yell. Esophageal intubation can turn the litmus paper yellow for a few breaths if patient has carbonated beverages in the stomach. This manifests as increased pulmonary blood flow and subsequent left ventricular overload since shunting occurs during systole. Lesions with similar pathophysiology include large ductus arteriosus and aortopulmonary window. In the first 24 hours after surgery, the hypertension is due to a catecholamine surge and should be treated with sympatholytics such as labetalol.
The student would also be able to appreciate the necessity of team-work cholesterol test last meal purchase 10 mg zetia overnight delivery, effective leadership and prudent resources management in Medical Practice cholesterol definition gcse cheap zetia. Course Duration the course in Family Medicine should last for a minimum of 2 weeks cholesterol chart by age buy 10 mg zetia. Course Outline Introduction to general practice cholesterol test pharmacy dublin discount 10mg zetia with visa, including the history of General Medical Practice and highlighting the need for the General Medical Practitioner in contemporary society Characteristics of Primary Care History of Medicine Concise and Precise history taking and prompt diagnosis cholesterol purchase zetia with mastercard. Therefore raise good cholesterol foods purchase cheapest zetia and zetia, the importance of its full integration into the undergraduate curriculum cannot be over emphasized. Pre-Clinical teaching of radiology should be encouraged right from the onset of training. At this level, a brief knowledge of the production of x-rays should be gained by the student and emphasis should be laid on basic radiological anatomy. Table 6:3 Instruction in Radiological Anatomy Gross Anatomy Radiological Anatomy Musculoskeletal System As demonstrated on plain X-rays. Gastro-intestinal Tract As shown in Barium Swallow, Barium Meal and Follow Through. The physiological basis of procedures in radiology should be stressed during lectures in physiology. Clinical Stage Introductory lectures at clinical level should cover areas such as x-rays production techniques and indications for various radiological procedures. At final examinations, a question or two should be incorporated in to each of the major papers. Film viewing sessions should form a prominent feature in oral examinations, in order to assess the clinical and practical acumen of the students. Course of Instruction Introduction/Production of X-ray and Film Processing Gastro intestinal tract radiology Liver, biliary tract, pancreatic radiology Chest X-ray: basic concepts. He should not only know what to ask for, but also the appropriate sequence of requests till radiological examination is concluded. Pharmacology, Applied Pharmacology and Therapeutics Aims and Objectives of Course General To introduce the medical students to the principles of drug treatment in diseased states To impart knowledge of the understanding of properties of drugs and the mechanisms by which they produce their effects in diseased conditions. Specific At the end of the course, the student should be able to 69 utilize the knowledge acquired to prescribe drugs or remedies for diseased states in man understand the pathological condition or altered physiological state from his knowledge of pathology and other clinical sciences prescribe appropriate drugs from his knowledge of pharmacology Duration of Course Instruction in pharmacology and applied pharmacology should be over a period of two academic years after the students have finished their studies in Anatomy, Physiology and Biochemistry. The course should be so organized that the students are gradually exposed to the study of drugs used in different disease states, as they progress through their clinical postings and have opportunity to see patients and study their management. This period may be divided into one academic year of basic principles of drug use in man and experimental animals followed by another year of clinical pharmacology during the rotation through the clinical and Community Health departments. Course Content the course should aim at providing the students with basic knowledge of drug action and extension of this knowledge to drug therapy. Systemic pharmacology should include wide areas of selected topics in different systems and organs. General Pharmacology the Scope of Pharmacology; Origin and Sources of Drugs; Routes of Administration of Drugs; Pharmacokinetics, Absorption of Drugs, Distribution of Drugs; Biotransformation of Drugs; Excretion of Drugs; Clearance and Half life of Drugs; Modes of Action of Drugs in Man; Compliance/Adherence Issues; Individual Variations; Interactions with other Drugs Concurrently or Previously Administered; Genetic Effects; Tolerance and Tachyphylaxis; Effects of Diseases; Drug Toxicity; Adverse Drug Reactions; Drug Dependence. Systemic Pharmacology Drugs Acting on the Alimentary System Vomitting-Antiemetics; ConstipationPurgatives, Ulcer Healing Drugs; Gastrointestinal Hormones-Pentagastrin, Secretin, Non-specific Antidiarrhoeal Drugs; Lactulose, Lipid Disorders-Cholestyramine; Pancreatin: Cholecystokinin Drugs Acting on the Respiratory System Oxygen Therapy; Bronchodilators; Asthma and Status Asthmaticus, Cough Suppressants; Mucolytic Agents; Respiratory Stimulants 70 Drugs Acting on Blood-Forming Organs Anaemia; Iron Deficiency and other Hypochromic Anaemias; Megaloblastic Anaemia; Iron; Cobalamins; Folates; Anticoagulants; Heparin; Coumarins; Indanediones; Fibrinolysis Fibrinolysin; Thrombus; Platelet Aggregation Inhibitors; Blood Lipid-Lowering Drugs Drugs Acting on the Cardiovascular System Heart Failure and its Drug Management, Anti-Anginal Drugs; Ischaemic Heart Disease and its Drug Management; Antiarrhythmic Drugs; Hypertension and its Drug Management; Vasodilators Drugs Acting on the Urinary System Diuretics; Alteration of Urine pH; Urinary Tract Infections; Renal Failure; Immunity and Immuno-suppressive Agents Antimicrobial, Antifungal and Antiviral Drugs and Drugs Against Protozoal Diseaseso Sulphonamides; o Antibiotics: Penicillins; Cephalosporins; Aminoglycosides; Lincomycin; Peptide Antibiotics; Drug Treatment of Tuberculosis; Miscellaneous Antibiotics: Vancomycin, Spectinomycin, Fusidic Acid, Other Synthetic Antimicrobial Drugs; Nalidixic Acid; Nitrofurantion; Drug Treatment of Leprosy o Antifungal Agents: Polyene Antifungal Antibiotics; Imidazoles; Miscellaneous Antifungal Agents o Antiviral Agents: Methiasazone; Idoxuridine, Cytarabine, Adenine Arabinsoside, Interferons; Humoral Immunoglobulins etc. Parathyroid Hormones; Thyrocalcitonin; Diabetes Mellitus; Insulin; Oral Antiglycaemics; Adrenocortical Hormones; Glucocorticoids; Mineralocorticoids; Hyperaldosteronism; Sex Hormones: Oestrogens; Androgens; Progestogens; Antagonists to Hormones. Pharmacoepidemiology and Pharmacoeconomics Essential Drugs List and Essential Drugs Programme; Rational Drug Use: Guide to Good Prescribing; Management of Drug supplies; Drug Revolving fund and user fees and how to recover costs that should have been paid by statutory exemptions; Drug utilization Monitoring by periodic Audit surveys. Practical Classes/Demonstrations A reasonable number of practical classes and demonstrations should be organized to make the students understand the nature of drug action and how drugs can affect organ systems. Sciences of Pathology Aims and Objectives A thorough understanding and application of the knowledge of Pathology, as a medical discipline, is a veritable foundation for acquiring good medical education. The aim of this course therefore is to inculcate this knowledge in the medical graduate. Scope of the Course the scope of subjects to be covered during the course of medical training is extensive and should include the following sub-disciplines: Morbid Anatomy and Forensic Pathology Post Mortem Examinations Bacteriological Examinations 72 Parasitology Virology Serology Immunology Haematology and Blood Transfusion Chemical Pathology Clinical Pathology Instructional Methods the undergraduate lectures, tutorials and practical training should be effectively carried out in departments of Clinical Pathology (including bacteriology and virology) and of Haematology and Blood Transfusion. The teaching/learning experience should be integrated with introductory tutorials and bedside clinical instruction in Medicine and Surgery; Obstetrics and Gynaecology; and Paediatrics. Undergraduate medical students should watch and participate in Post Mortem Examinations. They are expected to learn the technique of performing autopsy safely and should be taught the important ethical considerations involved. Even after the formal examination, the students will be expected to continue to learn clinical pathology in the context of their final clinical rotations where they will be expected to attend the clinic-pathological conferences organized jointly by the clinical pathology and the core clinical departments Examinations, which should be held at the end of the course of training, should comprise written, practical and oral formats, and for the medical student to satisfy the examiners, he/she must score a minimum of 50%. Provisions for re-sit examination should be available within 3 months of the initial examination. Advanced (Final Block Posting) Serum protein and disorders Lipid and Lipoproteins and disorders Trace elements and disorders Vitamins and disorders Dietary Fibres 74 Disorders of over-nutrition (Obesity, hyperuricaemia and gout) Disorders of under-nutrition (Marasmus and Kwashiokor) Introduction to Endocrinology Hypothalamus and Pituitary Disorders of Thyroid axis Disorders of Adrenal axis Disorders of Gonadal axis Chemical Pathology of Pregnancy Chemical Pathology of Hypertension Biochemical tumour markers and Chemical Pathology of Neoplasia Demonstration of the Assay of each Analyte in the Chemical Pathology Laboratory. Infectious Organisms Gram positive cocci: Staphylococcus and Streptococcus Gram negative cocci: Neisseria etc Gram positive bacilli: Corynebacteria, Listeria, etc Gram negative bacilli; Enterobacteriaceae (Lactose and non-lactose fermenters) Bacterial Diarrhoeal Diseases Typhoid and other septicaemias Malaria; Parasitic Blood infections. Systemic Infections/Hospital Acquired Infections Urinary Tract infections Central Nervous System Infections Soft Tissue Infections Endocarditis and Septicaemia Respiratory Tract Infections Opportunistic Infections; Control of Hospital Acquired Infections Principles of Chemotherapy Fungal Infection: dermatophytes, yeasts, dimorphic fungi, dermatitious fungi Amoebiasis; Tapeworm Infection; Schistosomiasis. Introductory (General Pathology) Introduction to Pathology; Role of Autopsy 77 Normal Cell, Causes of Injury; Cellular Adaptation; Cell Death Body Reaction to Injury; Tissue Healing and Repair Disturbances of Haemodynamics Genetic Basis of Diseases Cell Growth and Proliferation Mechanisms Neoplasia: Mechanism of Carcinogenesis and Tumour Biology; Metastasis; Classification of Tumours Disorders of Nutrition 2. Medical Ethics and Jurisprudence Objectives the course should familiarize students with the following: Major codes of ethics relevant to Medicine viz the Hippocratic Oath, the Physicians Oath or Geneva Declaration (1948, 1968) the Declaration of Helsinki (1964, 1975). Instructional Methods Teaching of medical ethics should start with the teaching of medical history during the first year of pre-clinical studies. From then on ethics should be taught throughout the period of training until graduation. Methods to be used include Modelling, Lectures, Case Studies, Tutorials and Seminars. At some stage there must be an examination which must be passed by all students before graduation Lectures There should be at least 10 hours of lectures during the course, covering: Principles of the philosophical basis of moral discourse. Practical Community Health Experience Students should be exposed to at least 2 months practical experience of working in the field in the community to learn the strategies for Primary Health Care Delivery to such a community Training in Management and Educational Methods For reasons which had been stated earlier, a good knowledge of the basic principles and practice of Management, Educational Methods and Educational Technology should form part of the undergraduate curriculum. In general courses of instruction and methods of assessment of student performance must lay emphasis on problem solving and practical skills required for the practice of medicine, and not mere recall, in keeping with the requirement for the young graduate to be able to assume independent responsibility soon after graduation. It is however the duty of the Medical and Dental Council to satisfy itself that the knowledge, skill and attitude derived from such a curriculum meet the minimum standards required by Council before recognition can be accorded to the professional qualifications obtained after undertaking the prescribed courses of this curriculum. The nomenclature for the degree programme in Dental Surgery shall be specified by the institution either as a Bachelor of Dental Surgery or, for institutions with approval from Council to run four-year post-baccalaureate programmes, Doctor of Dental Surgery. Selection of Students In practice, more often than not, the decision on the minimum level of general education required of students wishing to enter dental schools is not optimally related to the dental school curriculum, but to the general format of secondary school education in the country. This period of education should provide students with the foundation to undertake the biological and physical sciences of the dental curriculum. The following secondary school subjects are deemed prerequisite to dental education: Biology: Physics: Chemistry: Mathematics and English. Prospective dental students must pass the West African School Certificate or the Senior Secondary School Certificate Examination or any equivalent examination, with at least Credit level passes in the above five subjects. The candidates must have offered and passed courses at undergraduate level in the following: 83 Physics including Mechanics, Thermodynamics, Optics, Basic Principles of Electromagnetism Chemistry including Physical Chemistry, Organic Chemistry, Inorganic Chemistry and Chemical Thermodynamics Biological or Life Sciences including General Mammalian Anatomy and Physiology (Human or Animal) covering the Musculoskeletal, Haemopoietic & Haemostatic, Immunological, Neurological, Cardiovascular, Renal, Endocrine and Gastrointestinal Systems); Psychology (Human Psychology and Basic Human Behaviour); General Biochemistry (including protein chemistry and the chemistry of other biomolecules, cellular metabolism and molecular biology); at least one of a selection of courses in microbiology, genetics, molecular genetics/biology, neuroscience, nutritional sciences, pharmacology, toxicology, botany, biology or zoology. The selection of the students should take into consideration the academic performance of candidates vis-a-vis the requirements of the future practitioners of dentistry. A minimum of 10 and a maximum of 30 annual intake of students are recommended, provided the admitting Institutions can cope in terms of academic staffing and infrastructural provisions. Curriculum Planning the planning and evaluation should be designed in such a way that there should be clear-cut objectives which must be evident and should be evaluated from time to time. In addition, the peculiar requirements of dental training demands that the additional physical facilities and personnel described in this chapter be made available. Academic Physical Facilities the standard of training given in a Faculty of Dentistry depends, among other factors, on the availability of physical facilities specifically designed and built for dentistry. It is possible that some of these facilities may exist within a College of Health Sciences, and be shared with another Faculty such as the School of Medicine. In addition to the lecture theatre/auditorium mentioned above, a minimum of 3 lecture halls, each large enough to accommodate a minimum of 30 students are mandatory. Research Laboratory It is desirable to have a common research laboratory for academic staff in the School of Dentistry. There should be one teaching laboratory fully equipped for prosthetics and another for Crown and Bridge. The 85 requirement of such a laboratory must meet the needs of the various cadres who will work there, such as: Lecturers in Prosthetics, Conservation, Orthodontics etc Dental Technology Instructors with expertise in different specialties. General Facilities for Professional Training the clinical facilities and requirements for professional training in dentistry are both extensive and expensive and to a large extent limited by the financial resources available. These facilities, a well-conceived curriculum and an adequate complement staff are all essential for a creating an environment conducive to learning. While variations of the facilities may occur from one institution to another, the minimum shall be the following: Dental Operatories Laboratories for the production of dental prostheses Laboratories for routine clinical investigations Radiological facilities Theatre facilities Instrument Storage Sterilization facilities Accidents and Emergencies Clinic In-patient beds Medical Records Department Pharmacy Unit for the Dental Hospital Phantom Head Operatories Dental Operatories these constitute the most important clinical facilities in a School of Dentistry. These operatories, equipped with instruments and materials, are used by the students for treatment of their patients, under the supervision of members of staff. The number of operatories should be such that there is one for two clinical students undergoing clerkship in each department. It should also allow easy supervision of students by staff and be sufficiently roomy to allow free movement of staff and students. Laboratories for Production of Dental Prostheses There should be one production laboratory for prosthetics and another for Crown and Bridge. Laboratory for Routine Clinical Investigations There should be an adequately equipped Oral Pathology laboratory to carry out investigations relevant to dentistry. Theatre Facilities There should be one theatre attached to the dental school for out-patient dental care under conscious sedation or general anaesthesia. There should also be a main theatre within the Teaching Hospital Complex for major oral and maxillofacial surgical operations. Instruments Storage and Sterilization Facilities There should be a main store to provide materials and instruments for the dental hospital Sterilization of instruments can either be done centrally or in units. In either case, the necessary storage space, work-top space and accommodation sterilizers must be provided. Accidents and Emergencies Clinic Within the dental hospital, there should be an Accidents & Emergencies Unit which should be opened 24 hours. In-Patient Beds There should be a clearly defined ward-space for the in-patient management of dental and maxillofacial patients. The bed complement shall be such as to offer clinical teachers the facilities to teach hospital dentistry. Whilst it is realized that, ordinarily, the bed complement for a dental hospital is not very large, it is still important that the minimum complement be equitably distributed for male, female and paediatric occupancy. Medical Records the medical records are important for: Proper care of patients Research database Medico-legal reasons the facilities should include a Records Department, which must be located within the dental hospital, and be manned by trained health records officers. The department must have a registration area, a filing section equipped with appropriate cabinets and racks, as well as a records library. Pharmacy Unit There should be a small pharmacy unit within the dental school, with a proper complement of registered pharmacists. Phantom Head Operatories There should be one complete phantom head with accessories for each pre-clinical student. General Infrastructure for a Dental School Dental equipment are highly sensitive to fluctuations in voltage of electric power supply and to the presence of particles in water. They cannot function without the following: An uninterrupted supply of electricity of steady voltage Particle-free pipe-borne water with adequate pressure head Therefore, a stand-by generator or as well as an adequate overhead water storage tank are mandatory. The failure of a lone compressor would mean a complete paralysis of the operation of the dental hospital. Therefore, in the installation of dental operatories, there should be a functional stand-by compressor. Since dentistry as a profession is equipment-intensive, it is mandatory to have a team of equipment technicians for routine maintenance of all the equipment. Good access roads as well as internal and external communication facilities are necessary. Specialized Equipment Pre-Clinical Dentistry Each student shall have one complete phantom head unit with its accessories for operative techniques. He shall also have for prosthetic techniques a Dental Motor with its hand piece and other accessories Clinical Dentistry There should be complete dental operatories with accessories; each clinical department shall have at least one dental operatory for two clinical dental students doing their clerkship in that department. Library and Information Resources Since the effectiveness of teaching is very much dependent on active research, facilities for basic and clinical research are essential components of a Faculty of Dentistry. There should be a well-equipped dental library, as part of an existing College of Medicine Library, with sufficient reading space and adequate supply of up-to-date journals, 88 periodicals and referenced textbooks. Human Resources Academic Staff Academic staffing is a major and critical determinant for the achievement of high standard of training.
One study showed a statistically significant reduction in number and volume of transfusions in preterm infants treated with erythropoietin crestor cholesterol medication side effects order zetia canada. Additionally reticulocyte counts were higher with a higher hematocrit value at the end of the study in treated patients [12] cholesterol types cheap 10mg zetia with mastercard. Erythropoietin appears to be a safe and important part of a conservative transfusion practice in neonates cholesterol levels explained generic zetia 10 mg overnight delivery. Only the latter of these were concerning for increased oxygen demand and oxygen debt that would be treated by increasing the hemoglobin level [15] cholesterol test at walgreens generic 10mg zetia mastercard. Bateman et al cholesterol test dublin generic zetia 10mg visa, looked prospectively at 977 children admitted to an intensive care unit cholesterol from foods order zetia now. Children who did receive a transfusion had longer days of mechanical ventilation, increased nosocomial infection and increased mortality. Interestingly, the most common reason for transfusion was low hemoglobin and the average pre-transfusion hemoglobin was 9. Hemoglobin levels were significantly lower in children in the restrictive arm during the study (8. There was no difference in the rate of new or progressive multiple organ dysfunction between the two groups (12% in each 220 arm). This study added support to the theory that children will tolerate a more restrictive transfusion threshold without an increase in adverse events, similar to the results seen in adults [1]. Overall, children appear to have better outcomes with a more restrictive transfusion protocol. Set transfusion thresholds of 7 g/dl similar to adult trials appear to be tolerated well in the pediatric population although the diverse patient population seen in pediatric intensive care units prevents one from making a single threshold that is all inclusive. Certain subsets of patients, such as sickle cell patients who have better postoperative outcomes when transfused to a hemoglobin of 10 g/dl, require the surgeon to treat each patient individually and consider the underlying pathophysiology that is treated when deciding upon an appropriate transfusion threshold [17]. Transfusion of Platelets Transfusion of platelets and other factors typically follow the recommended guidelines from adult surgical practice. The normal platelet count of neonates and older children is similar to that seen in adults. These factors should be replaced prior to surgical intervention and routinely monitored after surgery to ensure hemostasis. Underdeveloped subependymal matrix and diminished coagulation cascade lead to subsequent rupture at the capillary level. Platelet levels should be kept at 100 9 9 x 10 in sick premature infants and at 50 x 10 in more stable patients [23]. No standard guidelines exist and there is some institutional variability in protocols. However, one should consider transfusion to this level and possibly higher in the face of active bleeding [23]. Other clinical scenarios should following guidelines and practical application that is seen in adult patients. Transfusion Reactions There are several types of tranfusion reactions (see Table 2). A study evaluating 2509 transfusions in 305 pediatric intensive care unit patients revealed 40 acute transfusion reactions (1. Febrile nonhemolytic reactions occur in children who have previous exposure from transfusion or pregnancy. This reaction is due to acquired antibodies to proteinacious material in the blood. Pretreatment with antipyretic agents, anti-inflammatory agents or antihistamines may alleviate the symptoms. Typical symptoms may include fever, pain, tachycardia, hypotension, renal failure or hemoglobinuria. Graft-versus-host disease is a transfusion related condition that is seen in immunocompromised patients. This is especially important to pediatric surgeons in that many of their patients either are immunocompromised due to age and underdeveloped immune systems (neonates) or have acquired immunodeficiency due to chemotherapeutic regimens (oncologic patients). Associated mortality is extremely high, up to 90%, with most deaths occurring within one month. Irradiation of all blood products transfused in immunodeficient patients readily decreases this risk [22]. Otherwise, reaction supportive measures once it develops Allergic Recipient is allergic Can be as mild Diphenhydramine to donor blood; as skin rash or and/or support for usually seen in IgA anaphylaxis allergic reaction deficient recipients. Anticoagulation the American College of Chest Physicians recently published their updated recommendations on antithrombotic therapy in neonates in children [25]. This reference that provides updated recommendations and guidelines for management of thrombosis and neonates. One cannot stress enough their conclusion that there is a paucity of prospective randomized literature evaluating this condition in children and that the evidence supporting the majority of recommendations remains weak. Overall the incidence has been found to be about 10 fold lower in the pediatric population [26]. Evaluation of all pediatric discharges (<18 years of age and excluding routine newborn hospitalizations) revealed an overall incidence of 0. The rates were highest in children less than one year of age and over the time period study increased from 18. The neonate has an increased risk of venous thromboembolism due to its inherent prothrombotic hemostasis system. Levels of Protein C, Protein S, antithrombin are low compared to normal adult ranges. In addition to an immature hemostasis system, newborn infants can have inherited and acquired thrombophilic traits similar to adults. Management of thrombus utilizing unfractionated heparin remains the most common therapy. Initial loading dose of 75 units/kg followed by a continuous infusion of 28 units/kg is a safe starting point. If 227 needed, heparin reversal can be reversed with protamine (1 mg protamine for 100 units of heparin). To treat this entity, Heparin should be discontinued, and anticoagulation with other agents such as lepuridin and argatrobam should be done. Effects of transfusions in extremely low birth weight infants: a retrospective study. A Multicenter, Randomized, Controlled, Clinical Trial of Transfusion Requirements in Critical Care. Blood transfusion increases radical promoting non-transferrin bound iron in preterm infants. Association of necrotizing enterocolitis with elective packed red blood cell transfusions in stable, growing, premature neonates. Recombinant human erythropoietin stimulates erythropoiesis and reduces erythrocyte transfusions in very low birth weight preterm infants. Determinants of red blood cell transfusions in a pediatric critical care unit: A prospective descriptive epidemiological study. Anemia, blood loss, and blood transfusions in North American children in the intensive care unit. A new strategy for estimating risks of transfusion-transmitted viral infections based on rates of detection of recently infected donors. Current incidence and residual risk of hepatitis B infection among blood donors in the United States. Central venous catheter related thrombosis in children: analysis of the Canadian registry of venous thromboembolic complications. Introduction the alleviation of pain and anxiety is an important component of caring for the critically ill infant and child. Children in the intensive care unit require sedation and analgesia as adjuncts to procedures, facilitate mechanical ventilation, and assist with post-operative management and care. Adequate sedation and analgesia also have benefits of reducing the stress response and catabolism associated with surgery [2]. Minimal sedation (anxiolysis) is a drug-induced state whereby patients are sedate but able to respond normally to verbal commands. Moderate 232 sedation (conscious sedation/sedation/analgesia), is a drug-induced depression of consciousness during which patients are able to respond purposefully to verbal commands or light touch. Monitoring of respiratory status is important, as there is a potential risk of airway compromise. Deep sedation/analgesia is a drug-induced depression of consciousness during which patients cannot be easily aroused but respond purposefully after repeated verbal or painful stimulation. Patients lose the ability to protect their airway and require assistance for airway protection. Lastly, general anesthesia is a drug induced loss of consciousness during which patients are not arousable and are unable to protect their airway. Inadequate pain or sedation management comprised 70% of reported adverse events in mechanically ventilated patients [7]. Additionally the percentage of awake days was significantly less in continuous infusion [8]. The relationship between sedation regimens and mechanical ventilation has been examined in several studies. In the randomized control trial by Randolph et al, sedative use in the first 24 hours of weaning was found to strongly influence length of time on the ventilator and extubation failure in 233 infants and children [9]. Payen et al also found continuous intravenous sedation was an independent risk factor for prolonged mechanical ventilation after multivariate analysis [10]. Another review highlighted prospective studies that demonstrated a significant reduction in rates of unplanned extubation following institution of a sedation algorithm [11]. The best practice recommendations included establishment of a sedation protocol and regular assessment of level of sedation to help reduce the rates of unplanned extubations, however a specific algorithm or sedation assessment tool was not identified [11]. Hartman, et al published a systematic review of pediatric sedation regimens in the intensive care unit in Pediatric Critical Care Medicine. Thirty-nine studies were included in the review, representing 39 sedation algorithms and 20 scoring systems used to evaluate level of sedation. Although sedation regimens have been used extensively across neonatal and pediatric intensive care units, the data are lacking as to the appropriate dosing, safety and protocols for use [12]. Side effects include respiratory depression, nausea, vomiting, delayed gastric emptying, delayed intestinal motility, pruritus, constipation, miosis, tolerance, and physical dependence. Fentanyl [13] 235 Clinical characteristics: 100 times more potent than morphine. Half life 8 hours Precautions: o glottis and chest wall rigidity following rapid infusion of > 5mcg/kg o bradycardia 3. Methadone [13] Clinical indications: used to treat or wean opioid addicted or dependent patients. Codeine [13] Clinical effects: inactive until metabolized in liver by cytochrome P450 2D6 into morphine. Children with ultra-rapid metabolism for this drug can have higher than normal doses of converted morphine in their system 10% of children are poor metabolizers and will experience less analgesia 5. Meperidine [13] Metabolized into normeperidine, which is toxic metabolite that can accumulate in patients with liver disease and cause seizures. Clinical effects include decreased cerebral metabolism and blood flow, sedation, hypnosis, anxiolysis, anticonvulsant activity, anterograde amnesia, muscle relaxation, dose dependent depression of breathing, and decreased tidal volume. Use of benzodiazepines without opioid in presence of painful stimulus can cause hyperalgesia and agitation [13]. Half life 6 hours Side effects: respiratory depression and hypotension, tolerance. Lorazepam [2,13] Insoluble Clinical effects: Prolonged effects on mental status and respiratory drive. Prolonged elimination half life in infants (5-6 days) Precautions: May increase risk of intraventricular hemorrhage in premature neonates 2. Pentobarbital Clinical indications: Adjunct for sedation of intubated child when tolerance to benzodiazepines and opioids has occurred Dosing: Intermittent doses: 0. Mechanism unknown, however likely causes global neuronal depression, without side effects of respiratory depression, emesis, or hemodynamic alterations. Ketamine [2] 245 Dissociative anesthetic, used for induction agent for anesthesia, analgesic for conscious sedation, premedication before induction of anesthesia, sedative in critically ill. Infusions 1-2 mg/kg/hour Onset & elimination: 1-2 minutes, duration of action 15 minutes. Elimination 3-6 hours Precautions: can cause hallucinations, myotic jerking, hypersalivation, increased cerebral blood flow. They typically do not cause respiratory depression and associated with few withdrawal symptoms [2,13] 1. Oral or transdermal use as adjunct for sedation/analgesia in critically ill Dosing: 5mcg/kg/day; transdermal patches -100-300mcg Onset & elimination: 1-3 hours. Dexmedetomidine [13,15,17] Clinical indications: sedative and analgesic for mechanically ventilated patients in an intensive care settings and non intubated adult patients prior to or during surgical or other procedures. Majority of adverse events resolved without treatment or by decreasing dose of infusion the incidence of adverse effects did not increase with increased duration of 16 therapy. Rapid distribution in blood & rapid clearance, which is responsible for short duration of action. Local Anesthesia [13] these agents reversibly block the conduction of neural impulses along central and peripheral nerve pathways. Their use produce analgesia with minimal physiologic changes, therefore making them desirable for children undergoing procedures and post traumatic pain management.
Visible waves of gastric peristalsis may be seen passing across the upper abdomen cholesterol lowering foods south africa order zetia with visa. The pyloric tumour is usually easiest to feel either early in the feed or after the baby has vomited cholesterol free desserts purchase zetia master card. Assess degree of alkalosis at presentation and monitor correction prior to surgery cholesterol chart pdf buy zetia with a visa. Complications include perforation of the mucosa cholesterol ratio total hdl buy zetia 10 mg on-line, which is not serious provided it is recognized and repaired cholesterol medication ezetrol cheap 10 mg zetia free shipping, and wound infection high cholesterol foods beef order zetia 10mg on-line. Hydrogen chloride Renal compensation by loss from vomiting maximising bicarbonate reabsorbtion Results in Exchange of K+ and Na+ hypochloraemic for hydrogen ions in metabolic alkalosis distal convoluted tubule Fig. Diagnosis Chest X-ray: the majority of ingested foreign bodies are radio-opaque (coins). Button batteries in the oesophagus must be retrieved or pushed down into the stomach within a few hours of ingestion. Electrolytic ulceration of the oesophagus occurs rapidly and this may lead to perforation or stulation into the tracheal or aorta. Provided the child remains asymptomatic, surgery to retrieve the object should be deferred for several months. During the rst trimester of intrauterine development the foetal midgut transiently herniates into the umbilical cord. Malrotation is usually asymptomatic and only detected by contrast meal and follow through. Dilated stomach and duodenum (obstruction) No other air-fluid levels in the bowel, just a few small pockets of residual gas in small/large bowel Fig. The intussuscepted bowel becomes engorged, which causes rectal bleeding, and eventually gangrenous. Small bowel intussusception may occur as a post-operative complication in infants, typically following nephrectomy. The latter can be particularly dangerous as a tension pneumoperitoneum develops very rapidly. There is a recurrence rate about 10% whether the intussusception is treated radiologically or by surgery. Hepatic flexure Intussuscepted ileum becomes oedematous Blood vessels become with bleeding from the drawn into the mucosa intussusception Appendix drawn into the intussusception Small bowel obstruction Fig. The pathology of small bowel atresias varies (depending on how deep in the mesentery the vascular accident occurs) from an atresia in continuity with a mucosal membrane to a widely separated atresia with a V-shaped mesenteric defect and loss of gut (Fig. Lack of pancreatic enzymes results in meconium that is thick and viscous causing an intraluminal obstruction in the terminal ileum. Atresias in continuity Atresia with a gap Apple peel atresia Multiple atresias Fig. Dilated stomach Gas in duodenum and jejunum above atresia No gas in bowel distal to atresia Fig. Acute appendicitis begins with obstruction of the lumen of the appendix, often by a faecolith, and this causes vague central abdominal pain. Irritation of the peritoneum results in more severe abdominal pain localized to the right iliac fossa. The diagnosis of appendicitis is clinical and laboratory investigations are generally not helpful. The abnormality is immediately apparent at birth as a defect in the abdominal wall to the right of the umbilicus (Fig. Often this has to be staged using a silo because the abdomen is too small to accommodate the intestine. Exomphalos (omphalocele) the incidence of exomphalos is 1/3000 live births (see Fig. Infants should be repaired within a few weeks of diagnosis because the risk of incarceration is high. If the hernia cannot be reduced, emergency surgical exploration is necessary (but this is rare). Surgical treatment Many surgeons now perform a single stage pull-through in the neonatal period, managing initial intestinal obstruction with rectal washouts, but traditionally a 3-stage procedure is used. A dramatic gastroenteritic illness characterized by abdominal distension, bloody watery diarrhoea, circulatory collapse, and septicaemia. Anatomy the precise anatomy varies but the malformation can be subdivided into high and low/intermediate anomalies in males and females. This abnormality is termed intermediate because, although normal continence is to be expected, reconstruction involves division of a common wall between rectum and vagina. For this reason treatment involves a 3-stage procedure with defunctioning colostomy, anorectal reconstruction, and then closure of the stoma. Treatment involves a defunctioning colostomy within the rst 48hr of birth, reconstruction at a few months of age (most commonly involving a posterior sagittal anorectoplasty performed through a midline perineal incision), and then closure of the colostomy. This is a harmless reaction to the resolving umbilical stump and usually disappears by the 2nd to 3rd week. Treatment A persistent granuloma should be cauterized with a silver nitrate stick. Treatment involves surgical exploration of the umbilicus and excision of the duct with a small segment of ileum. Urachal remnants these are uncommon anomalies that present in infancy or early childhood. The urachus is an embryonic tubular connection between the bladder and the allantois that normally obliterates before birth. Testis has invariably infarcted and exploration is not necessary, nor is xation of the opposite testis. If the testis is disrupted surgical exploration and repair is necessary to prevent atrophy. If the blow is severe a urethral injury should be suspected and, if necessary, excluded by urethrography. These testes can be bought down into the scrotum with an orchidopexy performed through an inguinal incision. There is risk of malignant degeneration in an intraabdominal testis (1:70, compared with 1:5000 for normal testis). If the vas and vessels enter the deep inguinal ring (30%), an inguinal orchidopexy is indicated. If the vas and vessels end blindly at the deep ring (30%), then the testis has torted in utero and has resorbed. If a testis is seen inside the abdomen then it must be removed or bought down with a two-stage orchidopexy. The scrotum is well developed and the parents may notice that the testes are in place when the child is in a warm bath. The testes can be manipulated into the scrotum and will remain there until the cremasteric reex is stimulated. Characterized by an abnormal position of the external urethral meatus and is classied according to the location of the meatus (penis down to the scrotum; see Fig. The most common consequences of hypospadias are difculty urinating while standing and a cosmetic appearance of the penis that differs from that of other boys. Sexual function is not affected unless chordee, which may cause painful erections, is present. Surgery Surgical correction involves straightening of any chordee and reconstruction of the urethra to the glans. This may involve tubularizing skin from the prepuce so circumcision is contraindicated. Glanular Common the foreskin (60%) is deficient Coronal ventrally in Distal penile Uncommon hypospadias Proximal penile (30%) Penoscrotal Rare Scrotal (10%) Perineal Chordee is a ventral curvature of the penis associated with proximal hypospadias Fig. It is also very common for boys to complain of intermittent redness and discomfort from the prepuce. This is rarely the result of bacterial or candidal infection, but simply a chemical irritation from urine under the foreskin. These symptoms are self-limiting and resolve during childhood without intervention. The paraphimosis should be reduced under general anaesthesia and circumcision scheduled a few weeks later to prevent recurrence. Balanitis/balanoposthitis Balanoposthitis is acute inammation of the glans and foreskin associated with a purulent discharge from the preputial orice. The commonest cause in boys is trauma, usually a fall astride injury to the perineum. Entrapment between the zip slide and the teeth is more complicated because the slider has to be prised off with bone cutters. Imperforate hymen An imperforate hymen usually presents within a few days of life with a lower abdominal mass, sometimes associated with urinary retention. The imperforate hymen can be seen bulging through the introitus and treatment consists of incising the hymen. Occasionally, an imperforate hymen is not detected in the newborn period and presents at puberty with p amenorrhoea or a painful lower abdominal mass from a haematocolpos. Treatment again comprises incision of the hymen and should be performed under general anaesthesia. Nappy rash and exposure to urine cause a chronic irritation of the fragile labia which adhere. Labial adhesions cause no symptoms, but they are a major source of anxiety to parents. Topical application of oestrogenic cream for 2wks will result in separation of most adhesions but occasionally gentle separation under anaesthetic may be necessary.
Order genuine zetia. सिर्फ 20 दिन में कोलेस्ट्रोल triglycerides को जड़ से खत्म करे हार्ट ब्लॉक से छुटकारा पाएं..
References
- McKenna PH, Bauer SB: Bladder augmentation with ureter, Dialogues Pediatr Urol 18:4, 1995.
- Duenas-Gonzalez A, Zarba JJ, Patel F, et al. Phase III, open-label, randomized study comparing concurrent gemcitabine plus cisplatin and radiation followed by adjuvant gemcitabine and cisplatin versus concurrent cisplatin and radiation in patients with stage IIB to IVA carcinoma of the cervix. J Clin Oncol 2011;29(13):1678-1685.
- Mercuri E, Clements E, Offiah A, et al. Muscle magnetic resonance imaging involvement in muscular dystrophies with rigidity of the spine. Ann Neurol. 2010;67:201-208.
- Prins GS, Marmer M, Woodham C, et al: Estrogen receptor-beta messenger ribonucleic acid ontogeny in the prostate of normal and neonatally estrogenized rats, Endocrinology 139(3):874n883, 1998.
- Di Stasi SM, Giannantoni A, Massoud R, et al: Electromotive vs passive diffusion of Mitomycin C into human bladder wall: concentration-depth profile studies, Cancer Res 59:4912n4918, 1999.
- Timberlake MD, Corbett ST, Costabile RA, et al: Identification of adolescent and adult patients receiving pediatric urologic care and establishment of a dedicated transition clinic, J Pediatr Urol 11(2):62, e1ne6, 2015.
- Fisher WA, Rosen RC, Eardley I, et al: Sexual experience of female partners of men with erectile dysfunction: the female experience of menis attitudes to life events and sexuality (FEMALES) study, J Sex Med 2(5):675n684, 2005.
