Proscar
Hanna K. Sanoff, MD
- Assistant Professor of Medicine
- Division of Hematology and Oncology
- Lineberger Comprehensive Cancer Center
- University of North Carolina School of Medicine
- Chapel Hill, North Carolina
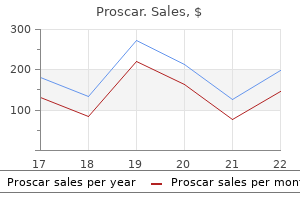
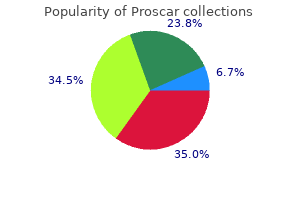
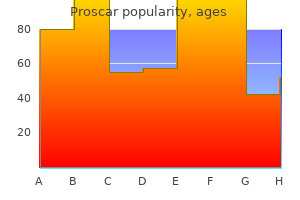
They observed that iliofemoral venous patency was significantly better and venous pressures mens health home workout buy on line proscar, leg edema anti-androgen hormone therapy for prostate cancer generic proscar 5 mg fast delivery, and postthrombotic morbidity were lower in Figure 1 androgen hormone chemotherapy generic proscar 5 mg otc. Endoluminal images after phlebotomy of the common patients randomized to venous thrombectomy prostate 8 ucsf buy proscar 5mg without prescription. Integrating mechanical Neovascularization techniques with catheter-directed lysis has reduced the Abundant Chronic dose of the plasminogen activator prostate wellness cheap proscar 5mg amex, reduced the length of collagen inflammation the hospital stay mens health face care buy 5mg proscar with visa, and improved the efficiency of thrombus removal. Hematoxylin/eosin staining showing abundant collagen, neovascularization, recanalization, and inflammation restored to the femoral vein ure 3C), common femoral in the common femoral vein. The patient had persistent obstruction of the common iliac vein, which was corrected with a 16-mm bare-metal stent ure 3E). Posttreatment assessment of a patient with deep vein thrombosis treated by pharmacomechanical thrombolysis and stenting after unsuccessful anticoagulation. Photograph of a patient with severe acute phlegmasia cerulea dolens after 5 days of treatment with low-molecular-weight heparin (Panel A). Patency restoration to the femoral vein (Panel C) and the iliac venous system (Panel D) after pharmacomechanical thrombolysis. The patient had persistent obstruction of the common iliac vein, which was corrected with a 16-mm bare-metal stent (Panel E). At the 36-month follow-up, the physical examination was normal and the veins were patent with normal valve function (Panel F). Annu Rev postthrombotic syndrome after acute description of the tissue causing chronic Biochem. Vascular endothelial treatment of choice in acute iliofemoral thrombosis determine the risk of disease growth factor receptor-2: structure, venous thrombosis. Eur J leg in deep vein thrombosis and kinases Tie-1 and Tie-2 in blood vessel Vasc Surg. Catheterterm outcome after additional catheterpharmacomechanical thrombectomy directed thrombolysis for iliofemoral directed thrombolysis versus standard for treatment of symptomatic lower deep venous thrombosis improves treatment for acute iliofemoral deep extremity deep venous thrombosis. The positive impact of micronization on the pharmacological activity of purified flavonoid fraction has been demonstrated in both animal and clinical pharmacological trials. The use of plants and isolated phytochemicals for the prevention and treatment of various health ailments has been in practice for years. About 25% of the drugs prescribed worldwide are derived from plants and 121 such active compounds are currently in use. Flavonoids have been reported to chelate metal, inhibit enzymes, inhibit cellular proliferation, induce apoptosis, stabilize membranes, and scavenge free radicals. Flavonoids have antioxidant, anti-inflammatory, antiallergic, antibacterial, osteogenic, cytotoxic, antitumoral, hepatoprotective, antithrombotic, and antiviral pharmacological properties. The sun-dried oranges are then fraction (ie, diosmetin, hesperidin, linarin, and isorhoifolin; ground and hesperidin is extracted in powder form. This and an oxygenated heterocyclic skeleton that is composed review contains an overview of the pharmacological of two aromatic rings. To * fi fi fi fi date, more than 4000 flavonoids have been identified and Registered as: Alvenor, Ardium, Arvenum 500, Capiven, fi fi fi they are widely distributed in the leaves, seeds, bark, and Daflon 500 mg, Daflon 1000 mg, Detralex, Elatec, fi fi fi flowers of plants that constitute an integral part of the human Flebotropin, Variton, Venitol. The most important groups are the anthocyanidins, catechins, flavones, flavanones, and flavonols (Table I). Microcrystalline cellulose is an inert substance a bovine, ovine, or poultry origin; therefore, it is that is widely used as a binder and diluent in compatible with the Muslim religion and a gout many pills and tablets. Magnesium stearate and talc are inert substances taken orally, and as a result, it is often used as a used as lubricants. Such inflammatory processes start with In humans, elimination of micronized diosmin is relatively inappropriate activation of leukocytes in the veins. A total of 41 C0s patients were enrolled, and, compared with contralateral healthy legs. For most measurements, the results obtained vein diameter was greater in the subgroup of patients with four tablets were significantly reinforced compared with transitory reflux compared with patients without reflux with those obtained with two tablets, but the effect was not (P<0. Additionally, vein diameter returned of 600 mg of diosmin is probably insufficient. The only nonsignificant effects were for itching, intubation for 26 weeks, no deaths, changes in weight, or but the sample size was the lower (n<500). In this analysis, the incidence of adverse events mg/day for 4 months) or placebo (n=296; same process), was not significantly different in patients >70 years old or symptom intensity as assessed using a 10 cm-visual analog with concomitant diseases (ie, hypertension, atherosclerosis, scale decreased from 6. Benefits of the micronized purified flavonoid fraction on symptoms and quality of life of C3 and C4 patients. Despite a lack of homogeneity between studies, a Cochrane review of 44 controlled studies of venoactive Modified from reference 38: Rabe E et al. All other Hydroxyethylrutoside * causes of edema should be excluded to confirm its venous origin. Venous edema is described as sporadic, unilateral Ruscus extract or bilateral, and more frequently located at the ankle. An ideal treatment would rapidly and significantly reduce symptoms, Email: arnaud. Micronization enhances the protective analytical aspects of diosgenin: a concise biopharmaceutic drug classification: effect of purified flavonoid fraction report. Accessed 3-O-glucuronide as major metabolite of In vivo and in vitro glucuronidation of the February 23, 2016. Daflon 500: oral administration to healthy volunteers summary of product characteristics. Pharmacodynamic flavonoid fraction versus placebo on properties and therapeutic efficacy of 28. Study of the effects of S 5682 symptoms and quality of life in patients Daflon 500 mg. Damon M, Flandre O, Michel F, Perdrix the Russian multicenter controlled of venous valves. Analysis of the various procedures reperfusion injury by elevation thromboxane B2 release and histological used in great saphenous vein surgery in of microvascular pressures. Eur J Vasc Mechanisms in experimental venous disease: patient compliance and efficacy. Symptoms appear early in the progression of the disease and with time may be associated with clinical signs of increasing severity. It describes the multifactorial nature of the condition that leads to very different rates of progression in different patients Phlebolymphology. This 92 fi Risk factors for chronic venous disorders and Phleboscore Phlebolymphology Vol 23. The increase in valve thickness with age would the legs has been refuted because the majority of varices explain the age gradient seen in the incidence of venous appear during the first trimester of pregnancy when the thrombosis. Epidemiological studies, including the Basel study,31 remodeling of the venous wall and valves that affect both the Edinburgh Vein Study,9 and the study by Jawien et al6 its cellular component19-22 and its extracellular component, observed a relationship between obesity and varicose veins as observed by Bujan et al. In the Edinburgh showed a higher incidence of varicose veins in women Vein Study,9,26 the prevalence of varicose veins and chronic who were more likely to be obese than men. Cornu-Thenard et al studied the role of the family inversely associated with moderate disease in women. Regular movement one parent was affected, and 20% when neither parent when sitting for long periods was related to lower rates was affected. Abnormal static posture of the foot may account for Lifestyle factors improper emptying of the plantar venous pump while Smoking was found to be a risk factor for varicose veins walking. Since the venous pump of the human foot is the in the Framingham study,12 but only in men, not in women. In a recent study from the risk factors retained for constructing Phleboscorefi are Finland,37 the 5-year incidence of varicose veins in both summarized in Table I. Limbs that underwent a superficial or deep venous contralateral, but initially asymptomatic, limb in 5 years. In procedure remained stable or improved over time; those these patients, obesity, orthostatism, and noncompliance that underwent elastic compression alone had worsening with the use of elastic stockings were independent risk hemodynamic and clinical status. The risk of ulceration is related to the severity childhood to adulthood in subjects with healthy veins. Large varicosities However, the risks may also be increased in those who appeared in older subjects, often preceded by reflux in the smoke, are obese, and have restricted ankle movement and 17 reduced power in the calf muscle pump. The presence of the symptom of 96 fi Risk factors for chronic venous disorders and Phleboscore Phlebolymphology Vol 23. Version from November 2015, printed with the kind permission of Dr Philippe Blanchemaison. Multifactorial evaluation of the risk factors for chronic venous disorders in men. Symptoms Prefer an antifluid retention diet by drinking water, tea, and herbal tea Q2, Q3, and Q4 >6 and choosing vegetables known for their fluid elimination properties (artichokes, black radish, asparagus, leeks, etc). History that promotes occurrence of venous disease Medical history Monitor the appearance of your legs and symptoms related to fluid Q6, Q7, and Q9 >18 retention Q6 and Q9 >12 Women <27 Consult your doctor in the case of varicose veins and swelling Men <21 Problem with being overweight Improve your diet and eat a balanced diet depending on basal Diet metabolism Q10 and Q11 >8 Prefer fresh food and home cooking instead of commercially prepared food. Walk 10 000 steps daily (at least 1 hour of walking) to stimulate circulation Physical habits in the legs Q12, Q13, and Q14 >8 Stretch your legs even when seated and do not wear tight clothing, particularly at the waist and thighs 98 fi Risk factors for chronic venous disorders and Phleboscore Phlebolymphology Vol 23. It is time to act decisively with personal action (eg, exercise, healthy venous lifestyle), and, in case of signs and symptoms of venous disease, with medical management (phlebotropic drug treatment, compression stockings, etc). Prefer an antifluid retention diet by drinking water, tea, and herbal tea Symptoms and choosing vegetables known for their fluid elimination properties Q2, Q3, and Q4 >6 (artichokes, black radish, asparagus, leeks, etc) Women 27-54 Undergo lymphatic drainage. Men 21-42 Medical History If you do not have varicose veins or edema, monitor your legs regularly and Q6, Q7, and Q9 >18 have them checked by your vascular specialist Remember to eat a balanced diet depending on your basal metabolism. You need to stop the progression of the disease by medical management (phlebotropic drug treatment, compression stockings, etc) and maintain the results obtained by a lifestyle that promotes healthy veins. Prefer an antifluid retention diet by drinking water, tea, and herbal tea Symptoms and choosing vegetables known for their fluid elimination properties Q2, Q3, and Q4 >6 (artichokes, black radish, asparagus, leeks, etc) Undergo lymphatic drainage and/or pressure therapy. Actions to take by subjects presenting with chronic venous disorders or disease according to their Phleboscorefi results. Phleboscorefi 75116-Paris, France should help to more accurately identify the patients at risk of developing a more serious disease so that interventions can be offered at an early stage to those who will gain the most benefit. Risk indicators for of the lower limbs: guidelines according varicose veins: the Framingham Study. Oral contraceptives intake may be Prevalence of primary chronic venous 2007;46:331-337. Schultz-Ehrenburg U, Weindorf of sex-related and lifestyle risk factors in N, Von Uslar D, et al. Importance of Prevalence of varicose veins and chronic the familial factor in varicose disease. Lifestyle risk factors for lower limb venous reflux in the general population: Edinburgh Vein Study. Chronic venous disease progression epidemiological study in England and high degree of venous reflux during and modification of predisposing factors. For postthrombotic syndrome, duplex ultrasound can recognize specific anatomical abnormalities in the venous lumen, wall, and valves. Reflux can be easily diagnosed with duplex ultrasound, although some controversy is present concerning the extent of the reflux detected compared with descending venography. Before operative recanalization, duplex ultrasound can be used to determine the procedure, feasibility, expected permeability, and safest venous access site; evaluate suprainguinal venous segments and infrainguinal vessels to determine the landing zone; distinguish between postthrombotic syndrome, primary and congenital incompetence, or compression. Duplex ultrasound is currently used during postoperative follow-up after repermeation and stenting to determine Keywords: the permeability of the stented veins and recognize complications, such as deep vein refux; duplex ultrasound; thrombosis, residual stenosis, and intrastent intimal hyperplasia. Currently, duplex iliofemoral obstruction; postthrombotic ultrasound is the first-line examination for postthrombotic syndrome diagnosis, syndrome; venous stenting preoperative investigation, and postoperative follow-up because it provides relevant information for the operative management of obstruction and reflux, even if the preoperative assessment must be completed by venography and other instrumental investigations. Introduction Postthrombotic syndrome includes all of the venous signs and symptoms occurring after a deep venous thrombosis in the lower limb. Diagnostic and quantification of postthrombotic syndrome are based on clinical criteria, which are described For postthrombotic syndrome, duplex techniques offers appealing treatment possibilities, even for ultrasound checks for deep venous reflux at the femoral and patients without tissue damage, that are complementary to popliteal veins in patients who are standing and it uses a conservative treatments. Obstruction is resulting in low morbidity and mortality, and effective, with measured using an augmentation maneuver in patients in a high rate of technical success, patency, ulcer healing, and a supine position. Deep veins abnormalities In addition to a physical examination, duplex ultrasound is Anatomical abnormalities a mandatory and complementary assessment for patients At the acute stage of an obstructive deep venous presenting with chronic venous disease. Current guidelines thrombosis, the occluded vein appears as a dilated and strongly recommend using duplex ultrasound as the primary noncompressible vein with a clot filling the lumen of the diagnostic test for superficial venous insufficiency, suspected vein that is more or less echolucent according to the age of abdominal or pelvic venous pathology, postthrombotic the thrombus. For a nonocclusive thrombosis, the thrombus syndrome, or clinical suspicion of other forms of iliac or is usually floating in the lumen of a nondilated vein. Duplex the other hand, according to the depth of the veins, duplex ultrasound techniques have been extensively described in ultrasound is usually more precise for infrainguinal vein consensus documents. Basic duplex ultrasound examination of superficial veins includes assessing perforating veins and all of the saphenous vein junctions, trunks, and tributaries.
Allergen Immunotherapy is the repeated administration of allergens to patients for the purpose of providing protection against the allergic symptoms and reactions associated with exposure to these allergens prostate cancer 7 gleason buy proscar 5 mg lowest price. Immunotherapy (hyposensitization) may extend over a period of months prostate and bladder cheap proscar master card, usually on an increasing dosage scale prostate cancer 97 buy genuine proscar on-line. This is followed by a build-up of tolerance to the antigen (as evidenced by the higher doses that can be administered) and a decline in the symptoms and medication requirements prostate yourself before god buy proscar no prescription. Indications for allergen immunotherapy are determined by diagnostic testing appropriate to the individual needs of each patient and his/her clinical history of allergic diseases androgen hormone qui buy proscar 5mg with visa. At the same encounter mens health 60 day transformation review proscar 5mg lowest price, one dose from this vial is administered by one injection to the patient. Continuous glucose monitoring is a procedure in which a probe is inserted subcutaneously and attached to a monitor that is worn by the patient. The monitor records the glucose level for a 72-hour period at which time the probe is removed and the data are downloaded from the monitor. The patient records his or her insulin administration, meals, exercise, and any hypoglycemic events during the monitoring period, in addition to performing the usual finger stick glucose four times a day during the 3-day period. The service includes the initial hookup, calibration of the monitor, patient training, removal of sensor, printout of recording, and interpretation and report (95251). Neurology and neuromuscular procedures There are codes in the Neurology and Neuromuscular Procedures (95782-96020) subsection for sleep testing, muscle testing (electromyography), range of motion measurements. The codes in this subsection are usually reported by physicians who specialize in neurology (neurologists). A neurologist usually is a consultant to a physician who is seeking the advice and input of another physician concerning a patient with suspected neurologic problems. One of the specialized tests conducted in the neurology specialty area is sleep studies (95800-95811). If a physician performs only the professional component, modifier -26 is reported. During each of these stages, the rate and amplitude (height) of the brain waves are measured and compared with normal ranges. Certain neurologic conditions may be identified by the degree to which brain waves vary from normal ranges. Nerve conduction tests (95905-95913) are usually performed in conjunction with conventional motor nerve conduction studies of the same nerve and may include F-wave studies. An impulse generated at the stimulating electrode travels up the motor nerves to the motor neuron cell bodies in the spinal cord. The impulse then travels down the same motor nerves to the neuromuscular junction, and then to the muscle. Codes 95907-95913 are to be reported for each nerve tested, regardless of the number of stimulation sites along the sensory or motor nerve being tested. For a given patient, multiple motor or sensory nerve conduction codes may be assigned if multiple motor or sensory nerves are tested. Codes 95905-95913 report both sensory and motor nerve conduction studies with or without F-wave study and includes the interpretation and report. Code 95905 reports motor and/or sensory nerve conduction using preconfigured electrodes that have been customized to specific anatomic sites. To report sleep tests accurately, you must know the parameters and stages of testing. Additionally, many codes include a time component (such as 95803); so it is important to have the duration of the test stated in the medical record. Assessments of dysphasia, developmental testing, neurobehavior status, and neuropsychological test codes are also located in this subsection. According to the Sleep Testing Guidelines, polysomnography includes sleep staging with: a. Except for the basic developmental testing, the codes are defined on a per-hour basis. The results of all the tests are to be developed into a report that is included in the patient record. The employer requests the testing for all newly hired executives who will be working with highly sensitive government documents. Examples of assessments are clinical interview, behavior observation, and questionnaires. When the physician provides a significant separately identifiable E/M service, report the service with an appropriate E/M service reporting modifier -25. Bundled into the hydration services are local anesthesia, placing the intravenous line, accessing an indwelling access line/catheter/port, flushing at the end of the infusion, and all standard supplies. Codes 96360 and 96361 report intravenous hydration infusions that include the prepackaged fluid and electrolytes. If other than a prepackaged substance is used, that substance would be reported separately. If the drugs are mixed into the saline, then only the drug is reported and the saline is bundled into the cost of the drug and not reported separately. Included in these hydration codes are the physician supervision and oversight of the staff providing the service. Code 96360 reports 31 minutes to 1 hour of intravenous infusion hydration service and 96361, the add-on code, reports each additional hour. You can only report 96361 if the service is at least 31 minutes over the 1 hour that was reported with 96360. Therapeutic, prophylactic, and diagnostic injections and infusions Codes 96365-96379 report the administration of therapeutic, prophylactic, or diagnostic intravenous infusion or injection. Intravenous infusions are reported with 96365-96368 and are divided based on the time and type of infusion. The initial infusion is reported with 96365 (up to 1 hour), and each additional hour (over 30 minutes) is reported with 96366. Sometimes one infusion is provided followed by another infusion with a different medication (sequential infusions), in which case the initial infusion is listed first and the sequential infusion (add-on code 96367) is listed second. There are times when more than one infusion is provided at the same time, which is a concurrent infusion. A concurrent infusion is when there is one site and two lines infusing at the same time. To report therapeutic, prophylactic, and diagnostic injections (96372-96376), the physician must be present. Note that add-on code 96376 can only be reported when the service is provided in a facility. Therapeutic, prophylactic, and diagnostic injections are divided based on the method used for the administration. Subcutaneous and intramuscular injections are reported with 96372 in addition to a code to report the substance injected. For example, if the injection was a subcutaneous human rabies immune globulin, report 90375 for the substance and 96372 for the administration. The administration codes for vaccines/toxoids are reported with 90460/90461 or 90471-90474. Injections for allergen immunotherapy are reported with 95115/95117, not with therapeutic, prophylactic, or diagnostic injection codes. Intra-arterial (96373) and intravenous push (96374/96375/96376) are reported with therapeutic, prophylactic, and diagnostic injection codes. Chemotherapy administration Chemotherapy codes 96401-96549 report a variety of chemotherapy services. The Injection and Intravenous Infusion Chemotherapy codes (96401-96417) report subcutaneous/intramuscular, intralesional, and intravenous chemotherapy. Intra-Arterial Chemotherapy codes (96420-96425) report various forms of chemotherapy administered via the arteries. Other Injection and Infusion Services codes (96440-96549) report other types of chemotherapy, such as pleural (96440), peritoneal via an indwelling port (96446), and central nervous system (96450), in addition to refilling/maintenance of portable or implantable pumps or reservoirs (96521, 96522). There are two other sets of codes used to report chemotherapy services: Hydration (96360-96361) and Therapeutic, Prophylactic, and Diagnostic Injections and Infusions (96365-96379), which you learned about earlier in this chapter. Included (not reported separately) with chemotherapy infusion or injection codes 96401-96549 are the following: 1. Preparation of the chemotherapy agent(s) If other services are provided, they may be reported separately. The initial intravenous infusion (the treatment) is reported with 96365 and each additional hour of infusion, up to 8 hours, is reported with 96366. If a sequential (one after another) intravenous therapy is provided, the service is reported with 96367. When a concurrent (at the same time as another) intravenous therapy is provided the service is reported with 96368. A concurrent infusion is one in which multiple infusions are provided through the same intravenous line. If more than one substance is placed in the one bag, it is considered one infusate and one infusion. Any administration that is 15 minutes or less is considered a push, not an infusion. The administration of an initial or single intravenous push is reported with 96374 and each additional push is reported with 96375. The drug(s) or substance would be separately reported with the appropriate J code based on the amount and type. A patient will often receive hydration and ancillary medications before or after chemotherapy. Only one initial administration code can be reported for each encounter; other services are reported with secondary or subsequent codes. E x a m p l e A patient presents for a chemotherapy intravenous infusion session and is given a 40-minute hydration prior to chemotherapy reported with 96360. If the patient receives hydration before and after chemotherapy, calculate the entire time of hydration infusion. For example, a patient received 1 hour of hydration before chemotherapy infusion and 40 minutes of hydration after chemotherapy. Modifier -59 should be reported to indicate that hydration was provided prior to or following chemotherapy. Hydration provided at the same time as chemotherapy to facilitate drug delivery is not reported separately. The patient may also receive medications before and/or after chemotherapy, such as anti-nausea medications. These medications are reported in addition to the chemotherapy because chemotherapy is always the primary service. When the patient receives multiple intravenous infusions of medications and these medications are administered individually, each is reported separately; but if the medications are mixed together and given in one infusion, they are reported as one infusion. Code 96375 is an add-on code and is only reported with another code, such as 96413, Chemotherapy administration. The charges for the patients in the examples that follow would list the chemotherapy administration first, followed by the other service codes since the chemotherapy is the primary service. E x a m p l e After chemotherapy, a patient received Aloxi (J2469), Benadryl (J1200), and Decadron (J1100) in three separate infusions of less than 15 minutes (pushes). If the medications are all mixed together and administered in one infusion of less than 15 minutes, the J codes are reported along with 96375 fi 1. E x a m p l e A patient presents for chemotherapy and receives two pushes, one of Aloxi, 0. Chemotherapy with Rituximab, 100 mg, is administered for 3 hours by means of an intravenous infusion. Chemotherapy: 96413 (initial hour); 96415 fi 2 (2 additional hours); J9310 fi 1 (Rituximab). Chemotherapy is the initial infusion and the hydration and pushes are secondary/subsequent. If a significant identifiable office visit service was provided in addition to the chemotherapy administration, report that service with an E/M code, adding -25 to indicate the service was separate and significant. C O D I N G S H O T Chemotherapy administration codes (96549-96459) include the use of local anesthesia, initiating the intravenous therapy, access to an indwelling port, flush at conclusion, tubing/supplies/syringes, and preparation of the chemotherapy agent(s). The patient has breast cancer with metastasis (secondary site) to the bone of the spinal column. The nurse administers an injection of vitamin B, 900 mcg with12 direct physician supervision. The service was not significant enough to report a separate E/M code for the office visit.
The disease tends to occur auditory canals and middle ear cleft may appear stenotic prostate biopsy purchase on line proscar. The diagnosis is often made during evaluation for skeletal pain or incidentally on rouTreatment tine radiography man health boston proscar 5mg cheap. The histologic pattern in Paget disease is one phosphatase and urinary hydroxyproline are seen in associof alternating waves of osteoclastic and osteoblastic activation with clinical improvement androgen hormone testing discount proscar 5 mg line. Bone remodeling activity results in haphazard bony may document the arrest of bony lesions mens health australia 5 mg proscar amex. The early phase of the disease is dominated by bone resorption mens health urbanathlon sydney 2013 buy cheap proscar 5mg online, which is Surgical therapy for hearing loss and cranial neuropathy seen as lytic lesions mens health 300 workout 2014 generic proscar 5mg fast delivery. The marrow space subsequently fills in Paget disease should be considered only as the last with fibrovascular tissue, which later undergoes sclerosis. Surgery for conductive hearing loss in Paget disMultifocal areas of lysis and sclerosis within the temporal ease has not been satisfactory. Persistent symptomatic internal for a tortuous external auditory canal, constriction of auditory canal stenosis with sensorineural hearing loss the middle ear cleft, bony changes of the ossicular and facial nerve dysfunction following medical therapy chain, and demineralization of the otic capsule. Other cranial neuropathies due to foraminal stenosis are hemifacial spasm, trigeminal neuralgia, and optic atrophy. Osteogenesis imperPlain film x-rays of the skull may be diagnostic in Paget fecta has two major variants: congenita and tarda. The severe and life-threatening fractures sustained in utero only other diagnostic consideration is the pagetoid variant and in the peripartum period. In approximately 10% of cases, Paget broad range of clinical outcomes that span the range disease may present as a sharply delineated osteolytic skull from mild to lethal disease. There are two radiographic patterns: ple fractures, and early hearing loss is inherited through mosaic and translucent. There is an increase in osteocytes proliferative otic capsule dysplasia differentiate osteogenin both woven and lamellar bone, and a relative reducesis imperfecta tarda from cochlear otosclerosis. Conflicting theories have been proposed to explain the Treatment & Prognosis pathogenesis of this disease. Some advocate the hypothesis of osteoblast dysfunction that is responsible for immathe primary otologic symptom in osteogenesis imperfecta ture bone deposition; others advocate the hypothesis of is conductive hearing loss that occurs between the second increased osteoclast activity. The benefit of medical therapy with mal cell signaling due to defects of the extracellular calcitonin, sodium fluoride, and vitamin D is unclear. Clinically, the regulatory defect in bone turnover Surgical intervention with stapedectomy to improve conresults in pathologic fractures and hearing loss. There is Clinical Findings a greater tendency for bleeding and difficult footplate mobilization. Alternately, patients may choose to improve thus affects multiple organ systems, producing a broad hearing with an amplification device. Hearing loss in osteogenesis imperfecta Aharinejad S, Grossschmidt K, Streicher J et al. Auditory ossicle tarda can be audiometrically indistinguishable from otoabnormalities and hearing loss in the toothless mutation in sclerosis. However, osteogenesis imperfecta has an earlier the rat and their improvement after treatment with colonystimulating factor 1. Syndrome characteran otospongiosis-like focus, as seen in early otosclerosis, or ized by osteitis fibrosa disseminata, areas of pigmentation and diffuse changes within the otic capsule. Osteogenesis imperfecta: otologic and maxillofacial plication of osteogenesis imperfecta. Autosomal dominant osteopetrosis: an otoneurologic investigation of the two radiohave substantial overlap with those found in otosclerosis. Osteodystrophia fibrosa: report of a case rosteosis of the temporal bone: a histopathologic study. Surgical strategies are chosen by to have the diagnosis of a skull base tumor delayed the skull base surgeon based on approaching the tumor because of an incomplete work-up. By far, the majority with enough exposure to perform a complete and safe of skull base tumors are benign and can be successfully resection while minimizing neurologic morbidity. Tumors of the cerebellopontine angle and Meckel cave are not considered in this chapter General Considerations (see Chapter 61, Nonacoustic Lesions of the Cerebellopontine Angle). Surgical approaches to these three areas Paragangliomas (or glomus tumors) are tumors of paraganare numerous, and the nomenclature is confusing. To glionic tissue, which originally derive from the migration remove a lesion of the middle ear or mastoid, a masof neural crest cells during fetal development. These tissue toidectomy through a postauricular incision or a middle rests are distributed predominantly throughout the middle ear exploration through the ear canal is usually adequate. These cell clusters are innervated by toidectomy is performed along with skeletonization of the parasympathetic nervous system and function as the facial nerve, the sigmoid sinus, and the jugular bulb. A well-known, but rare, paraganglioma is the facial nerve out of its bony canal and rerouting it the pheochromocytoma. Permanent facial paresis or synkinesis can there are two main types of paraganglioma: glomus tymoccur. Surgical resection of a large jugulotympanic paraganglioma (Fisch Type A approach). Although the classic Fisch Type A approach involves closure of the external auditory canal and rerouting of the facial nerve, these procedures are not often required to resect even large jugular foramen tumors as shown in this example. Fisch Type B and C approaches (not shown) are not used to approach the jugular foramen, but instead are used to approach tumors of the infratemporal fossa, petroclival junction, and naF sopharynx. Good visualization of the petroclival junction, as well as the anterior brainstem, is obtained by this approach. Combined subtemporalLabbe retrolabyrinthine approach for resection of tumors of the petroclival junction. Excellent exposure of the Sigmoid entire brainstem from the posterior circle sinus of Willis to the jugular foramen is obtained. Together these bilateral glomus jugulare tumors and a 7% incidence of nerves are called the tympanic plexus, which consists of an associated carotid body tumor. In addition, another form of the disease has an autosomal dominant mode of transmission, and the Pathogenesis causative genetic defect has been localized to two separate loci: 11q13. Paragangliomas Paragangliomas are also associated with phakomaare slow-growing tumors, and metastases are extremely toses (neurologic diseases with cutaneous manifestarare. Within the skull base, they tend to extend through matosis, Sturge-Weber syndrome, tuberous sclerosis, fissures and foramina, vascular channels, and air cell tract and von Hippel-Lindau disease. Classification Approximately 1% of paragangliomas display functionally significant catecholamine secretion similar to a pheoThere are two main classification schemes for paragangliochromocytoma. Pathologically, the chief cell is the cell of mas of the temporal bone: Fisch and Glasscock-Jackson. Classic findings are clusters of chief cells, termed Zellballen, with a rich vascular plexus throughthe Fisch classification includes four main categories: out the entire tumor. Indeed, these tumors are highly vas(1) Type A (tumors limited to the middle ear), (2) Type cular and may bleed substantially during surgical excision. If the inner ear is invaded, a sensothe classification scheme of Glasscock and Jackson difrineural hearing loss will be found. Impedance audiomeferentiates between glomus tympanicum and glomus try will reveal a flat tympanogram if a middle ear mass is jugulare tumors. If the tumor is a glomus jugulare tumor that has extended the two most common presenting symptoms of a into the middle ear cavity, this bone will be eroded. In patient with a paraganglioma of the temporal bone are contrast, if the tumor is a glomus tympanicum tumor, conductive hearing loss and pulsatile tinnitus. There may be a semicircular canal fistula or the symptoms of sympathetic discharge, which may repretumor may be in close proximity to the fallopian canal, sent a functionally secreting tumor, such as tachycardia, particularly along the vertical segment. Moreover, extend anterior to the internal auditory canal or along the patient should be queried about any symptoms of the petrous portion of the internal carotid artery. These dysphagia or hoarseness, which may represent palsy of findings may affect the planned surgical approach. This pattern is due to flow voids from tion of the cranial nerves is indicated, with particular the large number of intratumoral blood vessels. This may occur directly if the tumor is usually done 1 or 2 days before surgical excision. This contacts the ossicular chain or indirectly if the tumor permits definitive diagnosis of the tumor by visualizing the blocks the eustachian tube, producing a serous middle tumor blush characteristic of such highly vascular tumors. Sensorineural hearing loss is uncommon In addition, the feeding vessels can be identified and embobut can occur if the tumor erodes the dense otic capsule lized to reduce blood loss during surgery. Paragangliomas of the temporal bone may cause facial nerve palsy (21%) by invading the nerve within the Differential Diagnosis temporal bone. Other temporal which the bony canal surrounding the nerve has been bone neoplasms that might involve the middle ear space eroded. It should be noted that rather than an isolated tumors; however, it does not eliminate viable tumor recurrent laryngeal nerve injury that causes vocal cord cells within the mass. Tumors have been known to paralysis (such as with a Pancoast tumor), the jugular recur even more than a decade after radiation therapy. Radiation therapy for paragangliomas of the temporal this is much more severe because the combination of a bone can be useful as a treatment for elderly patients lack of sensation to the upper larynx and vocal cord with symptomatic tumors or for patients who are paralysis puts these patients at extremely high risk of unwilling to undergo a surgical resection. Patients with functionally hypoglossal foramen in the occipital bone, anteroinfesecreting tumors need to be alpha-blocked with phentorior to the jugular foramen. Large paragangliomas that lamine before and during surgical resection to prevent extend inferiorly may affect the hypoglossal nerve. The life-threatening hypertension as the alpha-adrenergic patient may complain of worsening articulation, and hormones are released with tumor manipulation. For a glomus tympanicum tumor that is limited to the middle ear cavity, a simple middle ear exploration through E. After raising the sympathetic nerves to the head run from the supethe tympanic membrane, the tumor can be visualized rior cervical ganglion up along the internal carotid on the promontory. If the tumor is larger and the petrous portion of the internal carotid artery may extends into the mastoid air cells, a tympanomastoideccause an ipsilateral Horner syndrome with ptosis, miotomy with an extended facial recess approach may be sis, and ipsilateral facial flushing and sweating. This is a standard mastoidectomy via a postauricular incision with sacrifice of the chorda tympani F. Intradural to the facial nerve (the retrofacial air cells) can be tumors can grow within the cerebellopontine angle, resected after exposing the facial nerve along its vertical producing cerebellar dysfunction and imbalance, brainsegment to prevent injury to it. For glomus jugulare tumors, a larger surgical approach Tumors that grow superiorly or medially can affect is required. A tympanomastoid approach with Treatment an extended facial recess and complete skeletonization A. This approach is less acceptable for younger patients in the sternocleidomastoid and digastric muscles are sepawhom the tumor would be expected to grow substanrated from the mastoid tip so that the great vessels can tially during their life span. Superiorly, the sigmoid sinus is treatment of paragangliomas needs to be individualized occluded in the mastoid cavity, inferior to the junction based on the patient, the disease, and the physician. In either case, patients can wall of the sigmoid sinus and the tumor filling the usually regain the ability to eat within the first few sinus) is dissected from the posterior fossa dura and craweeks after surgery with swallowing therapy. There is usually substantial nerve palsy also can occur during tumor removal, bleeding from the entry point of the inferior petrosal although if the facial nerve is anatomically intact at the sinus to the jugular bulb during this process. After tumor removal, the mastoid nificant amounts of blood loss during the resection of cavity is often packed with fat harvested from the these tumors because of their highly vascular nature. Preoperative embolization is quite helpful in reducing Large glomus jugulare tumors, which extend anterithe amount of blood loss. Lateral skull base surgery for glomus tuthe facial nerve from the geniculate ganglion to the pes mors: long-term control.
Trusted 5 mg proscar. The Cases For and Against Circumcision.
Outpatient facilities are especially interested in the November or December edition of the Federal Register because Medicare reimbursements for outpatient services are usually published in one of those editions man health 8 news cheap proscar master card. Each year man health ru buy cheap proscar on-line, when changes to the various payment systems are proposed prostate cancer 20s order 5 mg proscar otc, those proposed changes are published early in the year prostate cancer keller williams purchase proscar 5mg without prescription, and a period of several months is offered to interested parties to comment and make suggestions on the proposed changes man health 4 all purchase proscar pills in toronto. The final rules are usually published in the fall editions and implemented in the following calendar year man health services discount proscar 5 mg fast delivery. Some addendums are particularly helpful to the coder because they list the active codes, noncovered codes, bundled codes, etc. Items 1 through 8 are always placed before the Final Rule, which is the official statement of the entire rule. Some provision was made for changes in the level on the basis of economic changes. The physician fee schedule is updated each April 15 and is composed of three basic elements: 1. A geographic adjustment factor to adjust for regional variations in the cost of operating a health care facility 3. Various financial protections have been designed and instituted on behalf of the Medicare beneficiary. The work component is identified as the amount of time, the intensity of effort, and the technical expertise required for the physician to provide the service. The malpractice component is identified as the cost of the medical malpractice insurance coverage/risk associated with providing the service. A relative value was established for a midlevel, established-patient office visit (99213) and all other services are valued at, above, or below this service relative to the work, overhead, and malpractice expenses associated with the service. Geographic practice cost index the Urban Institute developed scales that measure cost differences in various areas. An entire state may be considered a locality for purposes of physician payment reform. Beneficiary protection Several provisions in the Physician Payment Reform were designed to protect Medicare beneficiaries. As of September 1, 1990, all providers must file claims for their Medicare patients (free of charge). As of January 1, 2010, the Patient Protection and Affordable Care Act requires physicians and suppliers to submit claims within 12 months of the service date. Assigned claims submitted more than 12 months after the date of service will be denied payment. The Omnibus Budget Reconciliation Act of 1989 requires participating physicians to accept the amount paid for eligible Medicaid services (mandatory assignment) as payment in full. The provisions of the new limitations state that nonparticipating physicians and suppliers cannot charge more than the stated limiting charge. Limiting charge In 1991 and 1992, the limiting charge was specific to each physician. Beginning in 1993, the limiting charge for a service has been the same for all physicians within a locality, regardless of specialty. This includes global, professional, and technical services performed by a physician. The limiting charge is important because that is the maximum amount a Medicare patient can be billed for a service. For covered services, Medicare usually pays 80% of the allowable amount for participating physicians. The beneficiary is then balance-billed, which means that the patient is billed the difference between what Medicare pays and the limiting charge. E x a m p l e Limiting charge is $115 (Maximum charge) Allowable is $100 Medicare pays $80 (Medicare pays 80%) Patient is billed $35 ($20, 20% of $100, and $15, the remainder of the limiting charge maximum) Physicians may round the limiting charge to the nearest dollar if they do this consistently for all services. Uniformity provision Equitable use of the Medicare fee schedule requires a payment system with uniform policies and procedures. To prevent variation in interpretation, standard definitions of services are required. Adjustments Whenever an adjustment of the full fee schedule amount is made to a service, the limiting charge for that service must also be adjusted. These adjustments are identified on the physician disclosure, which is provided to all physicians during the participating enrollment period each year. Adjustments to the limiting charge must be manually calculated before submitting claims for all services in which a fee schedule limitation applies. Payments to nonparticipating physicians do not exceed 95% of the physician fee schedule for a service. Site-of-service limitations Services that are performed primarily in office settings are subject to a payment discount if they are performed in an outpatient hospital department. There is a national list of procedures that are performed 50% of the time in the office setting. These procedures are subject to site-of-service limitations for which a discount is taken on any service that is performed in a setting other than a clinic setting. If a physician provides this service in a hospital outpatient setting, the limiting charge will be less than that for the office setting. This is because the hospital will also be billing Medicare for the use of the room and the supplies. As an example, review the following rules regarding the assignment of just a few modifiers. If a surgeon performs more than one procedure on the same patient on the same day, discounts are made on all subsequent procedures, excluding add-on codes. Medicare will pay 100% of the fee for the highest value procedure, 50% for the second most expensive procedure, and 50% for the third, fourth, and fifth procedures. Each procedure after the fifth procedure requires documentation and special review to determine the payment amount. Discounting is why the order of the codes and the use of modifiers are so important! Third-party payers often follow different discount limits rules from those of Medicare. As in all other reimbursement issues, some non-Medicare carriers follow this pricing method, whereas others follow their own multiple-procedure discounting policies. Under the fee schedule, Medicare pays the same amount for surgical services furnished by several physicians as it pays if only one physician furnished all of the services in the global package. The policy is written with the assumption that the surgeon always furnishes the usual and necessary preoperative and intraoperative services and also, with a few exceptions, in-hospital postoperative services. In most cases, the surgeon also furnishes the postoperative office services necessary to ensure normal recovery from the surgery. Recognizing that there are cases in which the surgeon turns over the out-of-hospital recovery care to another physician, Medicare has determined percentages of payment if the postoperative care is furnished by someone other than the surgeon. These are weighted percentages based on the percentage of total global surgical work. For example: Preoperative care 15% Intraoperative service 70% Postoperative care 15% Again, become familiar with individual third-party payer policies, because some may not split their global payments in this manner. Physicians assisting the primary physician in a procedure receive a set percentage of the total fee for the service. Medicare sets the payment level for assistants-at-surgery at 16% of the fee schedule amount for the global surgical service. When two primary surgeons (usually of different specialties) perform a procedure, each is paid an equal percentage of the global fee. For cosurgeons, Medicare pays 125% of the global fee, dividing the payment equally between the two surgeons (each will receive the lesser of the actual charge or 62. No payment is made for an assistant-at-surgery when co-surgeons perform the procedure. For team surgery, a medical director determines the payment amounts on an individual basis. Modifiers -62 (Two Surgeons) or -66 (Surgical Team) would be appended to the procedure code. The amount paid by Medicare for a return to the operating room for treatment of a complication is limited to the intraoperative portion of the code that best describes the treatment of the complications. When an unlisted procedure is reported because no other code exists to describe the treatment, payment is usually based on a maximum of 50% of the value of the intraoperative services originally performed. Modifiers -78 (Return to Operating/Procedure Room for a Related Procedure During the Postoperative Period) or -79 (Unrelated Procedure or Service by the Same Physician or Other Qualified Health Care Professional During the Postoperative Period) would be appended to the code to more specifically identify that the service was a reoperation. But because Medicare is the largest third-party payer, it has the most comprehensive anti-fraud program. You must understand the specifics of this program because you will be submitting Medicare claims. Fraud is the intentional deception or misrepresentation that an individual knows to be false or does not believe to be true and makes it knowing that the deception could result in some unauthorized benefit to himself/herself or some other person. Fraud involves both deliberate intention to deceive and an expectation of an unauthorized benefit. By this definition, it is fraud if a claim is filed for a service rendered to a Medicare patient when that service was not actually provided. The fact is that most Medicare patients sign a standing approval, which assigns benefits to the provider and is kept on file in the medical office. Having a standing approval is convenient for the patient and for the coding staff. But a standing approval also makes it easy for unscrupulous persons to submit charges for services never provided. This circumstance also makes it possible for extra services to be submitted in addition to services that were provided (upcoding). Suppose, for example, a patient came in for an office visit and a claim was submitted for an inoffice surgical procedure that was not performed. C A U T I O N the most common kind of fraud arises from a false statement or misrepresentation made, or caused to be made, that results in additional payment by the Medicare program. The violator may be a physician or other practitioner, a hospital or other institutional provider, a clinical laboratory or other supplier, an employee of any provider, a billing service, a beneficiary, a Medicare employee, or any person in a position to file a claim for Medicare benefits. You will be the person filing Medicare claims so you have to be careful about the claims you submit. It is important to validate that the service was provided by consulting the medical record or the physician. Seldom do such perpetrators target just one insurer; nor do they focus exclusively on either the public or the private sector. Rather, most are found to be defrauding several privateand public-sector victims such as Medicare simultaneously. The plan is a published public document that provides the evaluation methods and approaches that will be taken the following year to monitor the Medicare program. For example, in the 2015 Work Plan, the following was listed as an item for review during 2015: T O O L B O X 1 1 Susan recently graduated as a medical coder and has been employed at Island Clinic for three months. Susan questioned the physician and he said that he just forgot to do the paperwork and asked her to send the claim to Medicare with a promise to complete the paperwork later. Complete the claim and send it in, and write a reminder to the physician to complete the documentation. Inform the physician that she cannot submit a claim without appropriate documentation in the medical record.
References
- Centers for Disease Control and Prevention: Control of smoke from laser/electric surgical procedures. National Institute for Occupational Safety and Health, Appl Occup Environ Hyg 14(2):71, 1999.
- Girman CJ, Epstein RS, Jacobsen SJ, et al: Natural history of prostatism: impact of urinary symptoms on quality of life in 2115 randomly selected community men, Urology 44(6):825n831, 1994.
- Stamatiou D, Skandalakis JE, Skandalakis LJ, et al: Perineal hernia: Surgical anatomy, embryology, and technique of repair. Am Surg 76:475, 2010.
- Premkumar MH, Colen JS, Roth DR, et al: Could scrotoschisis mimic an iatrogenic injury? A case report, Urology 73:795n796, 2009.
- Somford DM, Hamoen EH, Futterer JJ, et al: The predictive value of endorectal 3 Tesla multiparametric magnetic resonance imaging for extraprostatic extension in patients with low, intermediate and high risk prostate cancer, J Urol 190(5):1728n1734, 2013.
